Cancer is a disease of the body's cells. Normally cells grow and multiply in a controlled way, however, sometimes cells become abnormal and keep growing. Abnormal cells can form a mass called a tumour.
Cancer is the term used to describe collections of these cells, growing and potentially spreading within the body. As cancerous cells can arise from almost any type of tissue cell, cancer actually refers to about 100 different diseases.
How does cancer develop and spread?

As mutant cells (those with mistakes in their genetic blueprint) grow and divide, a mass of abnormal cells, or a tumour, is formed. In some cases, these cells will form a discrete lump, in other cases such as leukaemia, abnormal blood cells are in the body.
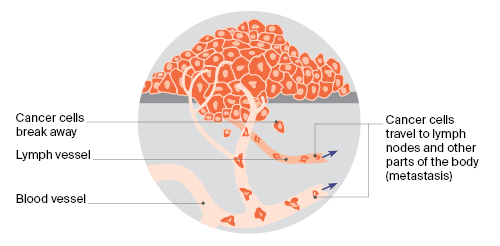
Cancer cells can break away from the mass (or tumour) and travel via the bloodstream or lymphatic system to different parts of the body. These cells can settle in other parts of the body to form a secondary cancer or metastasis.
Cancer can cause premature death because these secondary cancers stop parts of the body from working properly.
FAQ
What causes cancer?
We do not know all of the risks and causes of cancer. However, there are a number of chemical, physical and biological agents that have been shown to trigger the mistakes in the cell blueprint that cause cancer. These are called carcinogens and include tobacco, ultraviolet (UV) radiation and asbestos.
A number of cancers share risk factors:
- One in nine cancers, and one in five cancer deaths, are due to smoking.
- A study in 2010 found that about 2.8% of cancers are related to alcohol use.
- Many cancers occur as a direct result of dietary influences.
- Infectious agents or exposure to radiation can cause cancer (especially skin cancers from UV radiation).
- Some cancers result from inherited ‘faulty’ genes.
- Cancer is NOT caused by injury or stress.
How many Australians get cancer?
Cancer is a common disease and a major health problem in Australia today. At current rates, it is expected one in two Australians will be diagnosed with cancer by the age of 85.
An estimated 145,000 new cases of cancer will be diagnosed in Australia this year.
Cancer is a leading cause of death in Australia – almost 55,000 deaths from cancer were estimated for 2019.
Compared to 1982, around 25,000 more people die each year from cancer. This is due mainly to population growth and ageing. However, the death rate (number of deaths per 100,000 people) has fallen by more than 24%.
More than 66% of people diagnosed with cancer in Australia will survive more than five years after diagnosis.
What are the most common cancers?
The most commonly diagnosed cancer (excluding non-melanoma skin cancer) was prostate cancer, followed by breast, colorectal or bowel cancer, melanoma and lung cancer. There are more than 100 different types of cancer, but these five most common types account for 60% of all cases.
The most common cancers for men and women are listed in order below:
Men
- Prostate
- Bowel(colorectal)
- Melanoma
- Lung
- Head and neck
Women
- Breast
- Bowel(colorectal)
- Melanoma
- Lung
- Uterine
Which cancers cause the most deaths?
Cancer is a leading cause of death in Australia. The most common causes of cancer deaths are not necessarily the most frequently occurring cancers. While lung cancer is the fifth most common type of cancer overall, it is the leading cause of cancer death in Australians.
The most common causes of cancer-related death in men and women are listed in order below:
Men
- Lung
- Prostate
- Bowel(colorectal)
Women
- Lung
- Breast
- Bowe(colorectal)
Who gets cancer?
Anybody can develop cancer. One in two Australians will be diagnosed with cancer by the age of 85.
The risk of cancer increases with age – more than four times as many cancers are diagnosed in people over 60 years, as in those under 60. However, increased awareness about cancer, screening programs and early detection means that cancer is increasingly diagnosed in younger people – which means it is often found at an earlier stage and can be treated more effectively.
Can cancer be prevented?
With our current knowledge, we believe that at least one in three cancer cases can be prevented. Smoking, sun exposure, poor diet, alcohol use and inadequate physical activity are significant risk factors, which can be modified.
Not smoking, or giving up, is the single most effective strategy to prevent cancer. One in nine cancer cases, and more than one in five cancer deaths (over 7700 every year) are caused by cigarette smoking.
Protecting your skin from exposure to the sun's ultraviolet (UV) radiation is a simple and very effective strategy for preventing skin cancer. Around 12,000 Australian men and women are diagnosed with a melanoma each year, and an estimated 434,000 people are treated for one or more non-melanoma skin cancers. In 2016 there were nearly 2000 deaths from skin cancer in Australia, 1281 from melanoma and 679 from non-melanoma. Relative five-year survival rates for melanoma are 89% for men and 94% for women.
It is estimated that more than 4000 cancer deaths annually are due to poor diet, alcohol use, physical inactivity and having overweight. Again, these are deaths that can be prevented. See our preventing cancer section for more information on how you can reduce your cancer risk.
Is cancer contagious?
Cancer is not contagious. There is no reason to avoid people with cancer; in fact they will need your support and understanding.
We now know that some cancer genes are hereditary and so several family members may have the same or a related type of cancer. This is due to an inherited genetic disorder, not spending time together.
Human papillomavirus(HPV), a virus that causes 90per cent of cervical cancers, is contagious and is transmitted via sexual activity. However, cervical cancer itself is not contagious.
Does cancer always cause pain?
Some cancers cause pain, others do not. Some people experience pain as the result of tumour growth or advanced cancer, or as a side effect of treatment.
Pain relief is always made available to cancer patients suffering pain. Your doctor can advise you about what to expect and how the pain can be managed.
Is cancer always fatal?
Absolutely not. Advances in our knowledge about prevention, early detection and treatment mean that over 66% of people diagnosed with cancer today can be effectively treated. Almost nine out of 10 children with cancer are effectively treated and go on to live normal lives.
As we further our knowledge about the disease, survival rates are likely to increase. Your state or territory Cancer Council can provide further information and support for cancer survivors and people living with cancer.
Why do we have screening programs for some cancers?
Screening involves testing people who have no symptoms for the presence of early, potentially curable disease. At present national screening programs exist for breast cancer, cervical cancer and bowel cancer.
There is no national screening program from prostate cancer. Current evidence shows that the harms of population screening with the prostate specific antigen (PSA) test outweigh the benefits. Therefore, the PSA test does not form the basis of a population-based screening program (either alone or combined with digital rectal examination).
What tests should I have?
Women who are 25 to 74 years of age should have a cervical screening test two years after their last Pap test to check for cervical cancer. If your results are normal, you will then have the test every five years.
Also be on the lookout for any changes to your breasts; if you notice any lumps or other changes, talk to your doctor as soon as possible. Women over 40 are eligible for a free mammography screening every two years. We strongly recommend you are screened regularly if you are aged 50-74.
The National Bowel Screening Program is currently offered to free to all Australians aged 50-74.
A FOBT kit is automatically sent to your home.
Cancer Council Australia recommends that anyone interested in testing for cancer should speak with their general practitioner (GP).
How is cancer treated?
The type of cancer treatment or combination of treatments that a patient has depends on the type and stage of the cancer. The most common types of cancer treatment are surgery, chemotherapy and radiation therapy.
Some cancers can be cured if the tumour is detected and surgically removed before the cancer cells spread. Cemotherapy (anti-cancer drugs) and radiotherapy (radiation treatment) can also cure cancer, by killing cancer cells or stopping them from multiplying. Often these treatments are most effective when used together.
The main goal of treatment is to cure the disease, but if cure is not possible, different treatments may be used to control the cancer. New ways of treating cancer are always being developed and tested. In the future, we can expect to see a new range of 'designer drugs' that block the blood supply that tumours need to grow, correct the genetic defects that lead to cancer and assist the body's immune system to fight cancer.
What about treatment side effects?
Usually when you suffer a disease you feel symptoms such as pain, and the treatment makes you feel better. Unfortunately, with some cancers, you may not have experienced any pain or discomfort until the treatment begins.
Cancer treatments designed to kill cancer cells can have unpleasant side effects, such as nausea and vomiting, bowel problems, tiredness, hair loss and scalp problems, and effects on nerves and muscles.
Before beginning treatment, it is best to be aware of the possible side effects and changes that your body may go through, and ways of managing or reducing them.
How do I decide about treatment?
Sometimes, making decisions about your treatment can be very hard. It may be even harder when you know that the treatment is aimed at relieving and controlling symptoms rather than curing the cancer.
Once you have discussed treatment options with your doctor, you may want to talk about your options with your family or friends, nursing staff, the hospital social worker or chaplain, or your spiritual advisor. Talking it over can help you to sort out what course of action is right for you. In most cases it is safe to delay treatment a few days or a week or so, but you should not put it off longer.
Should I take part in clinical trials?
Your doctor may suggest that you take part in a clinical trial.
Doctors conduct clinical trials to test new or modified treatments and see if they are more effective than existing treatments.
Clinical trials are an essential part of the quest to find better treatments for cancer.
Hundreds of thousands of people all over the world have taken part in clinical trials that have resulted in many improvements to cancer treatment. All trials are approved by an Ethics Committee.
To help you make an informed decision about joining a clinical trial, your doctor will discuss the trial and its implications for you. If you join a 'double blind' clinical trial, you will be given either the best existing treatment for your condition or a promising new treatment. Treatments are randomly assigned, so neither you nor your doctor knows which treatment you are being given.
If you do join a clinical trial, you have the right to withdraw at any time. Doing so will not jeopardise your cancer treatment.
What about complementary therapies?
Many people with cancer consider complementary therapies in addition to treatment recommended by their doctors.
Complementary therapies are supportive therapies used to complement mainstream treatments. These are often recommended by your doctor or another health professional, not to cure disease, but help control symptoms and improve wellbeing. Examples include massage therapy, yoga, meditation, herbal teas and acupuncture.
What about alternative treatments?
There are many ‘alternative therapies’ that are promoted as cancer cures. They are unproven because they have not been scientifically tested,or were tested and found to be ineffective. If alternative therapies are used instead of evidence-based treatment, the patient may suffer, either from lack of helpful treatment or because the alternative treatment is actually harmful.
If you are thinking about using a treatment that is not an evidence-based medical treatment, make sure you carefully consider and investigate the claims being made. Look into the evidence for those claims, the credentials of the people or organisation promoting the treatment, the costs and the potential risks of delaying conventional treatments.
The American Cancer Society recommends the following checklist to identify treatments that might be questionable:
- Is the treatment based on an unproven theory?
- Does the treatment promise a cure for all cancers?
- Are you told not to use conventional medical treatment?
- Is the treatment or drug a ‘secret’ that only certain providers can give?
- Does the treatment require you to travel to another country?
- Do the promoters attack the medical/scientific establishment?
If the answer to any of these questions is 'yes', you should carefully consider whether the proposed treatment is of any value.













