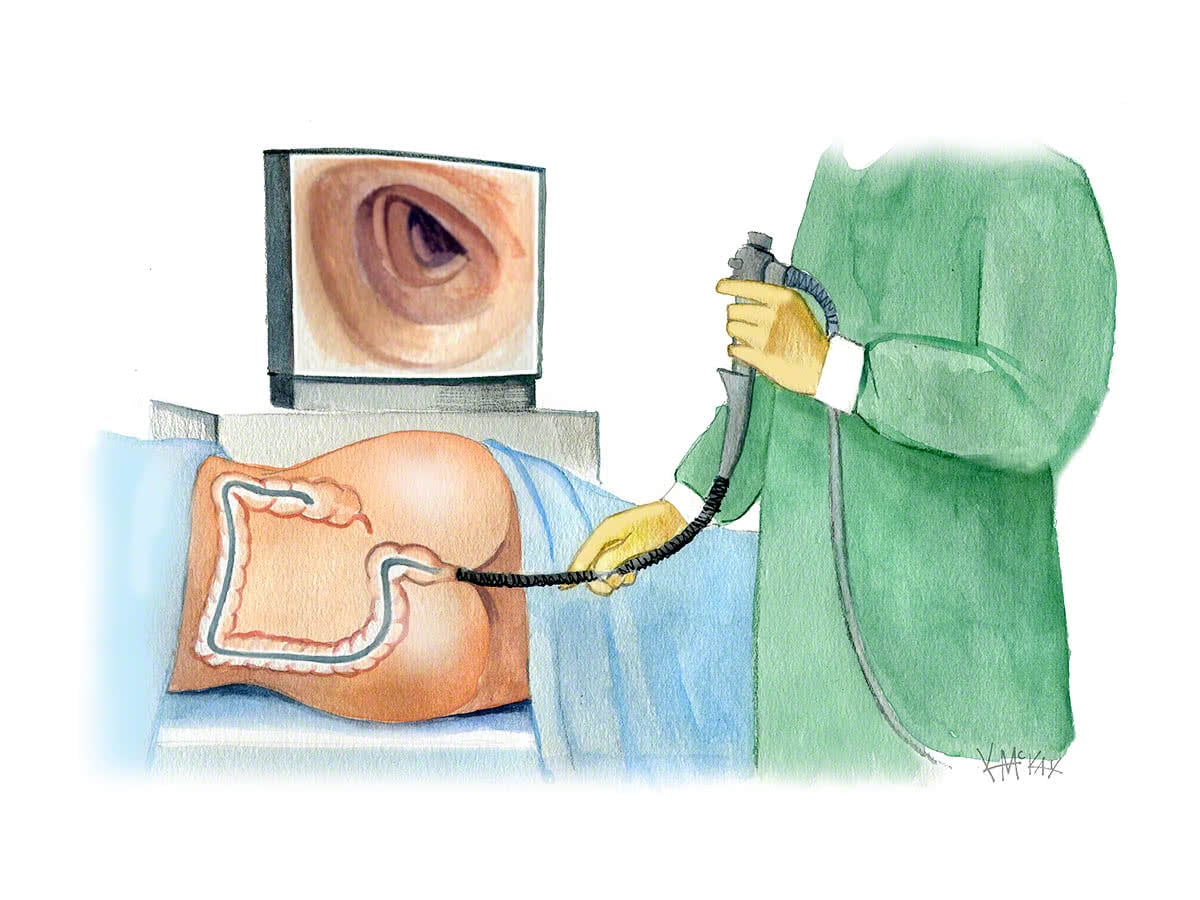
Colonoscopy is a simple day-stay procedure performed under sedation. It involves the passage of a flexible tube (colonoscope) about the thickness of a pen into the colon (also called the ‘large intestine’) via the back passage (anus) to allow for careful examination of the entire colon.
When is colonoscopy indicated?
Colonoscopy is performed to diagnose or treat a number of conditions of the colon, including altered bowel habit, constipation, rectal bleeding, or a positive faecal occult blood test (FOBT). It is also indicated in those with a family history of colorectal cancer, or previous polyps.
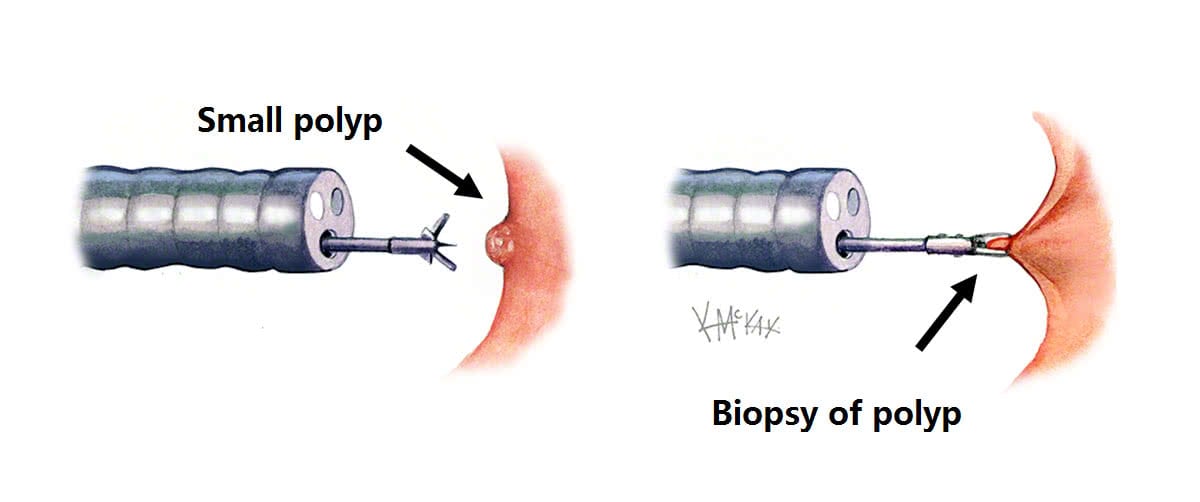
As well as giving better images than x-ray (barium enema or CT) of what the colon looks like from the inside, colonoscopy also allows for the removal of polyps (polypectomy) or biopsies of the colon. This is a painless procedure done while sedated that avoids the need for major surgery and protects against cancer.
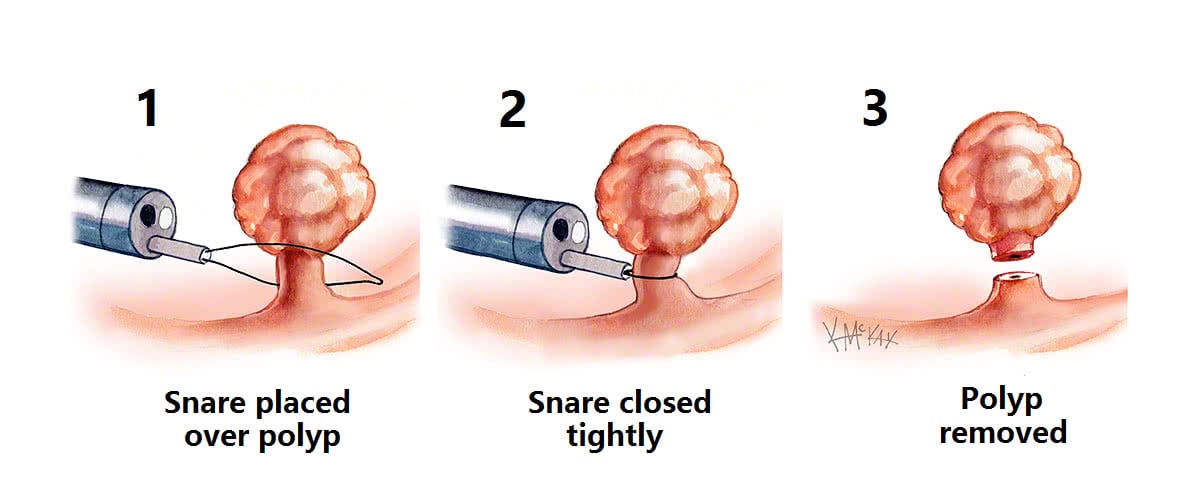
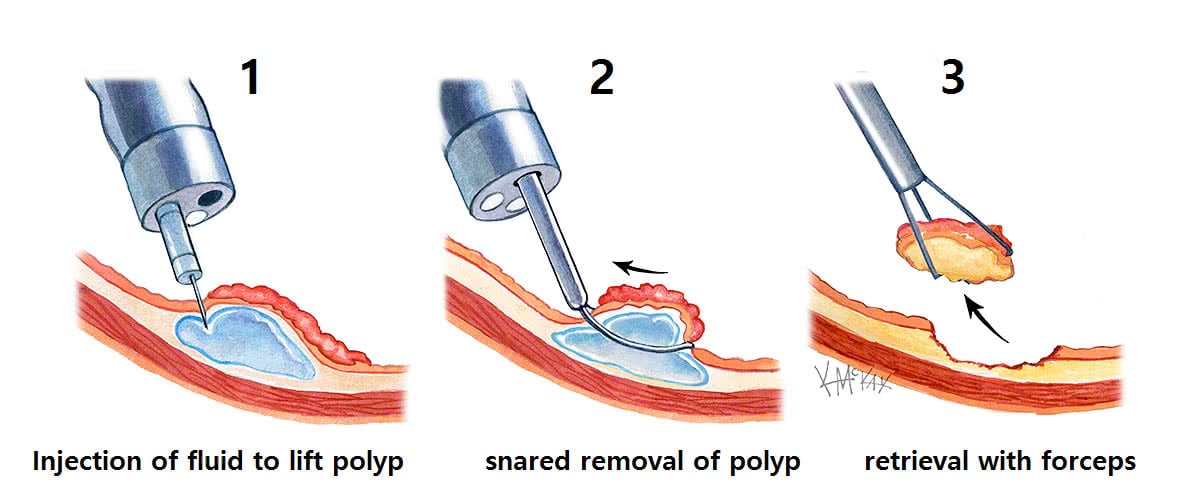
For polyps larger than 5mm, polypectomy is performed by passing a wire loop through the colonoscope and snaring the base of the polyp, which is then electrocauterised with the polyp then retrieved (Figure 3). This process is painless to the patient.
Endoscopic surgery includes techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) which are often needed for Polyps larger than 1.5cm. (Figure 4.)
Why perform a polypectomy?
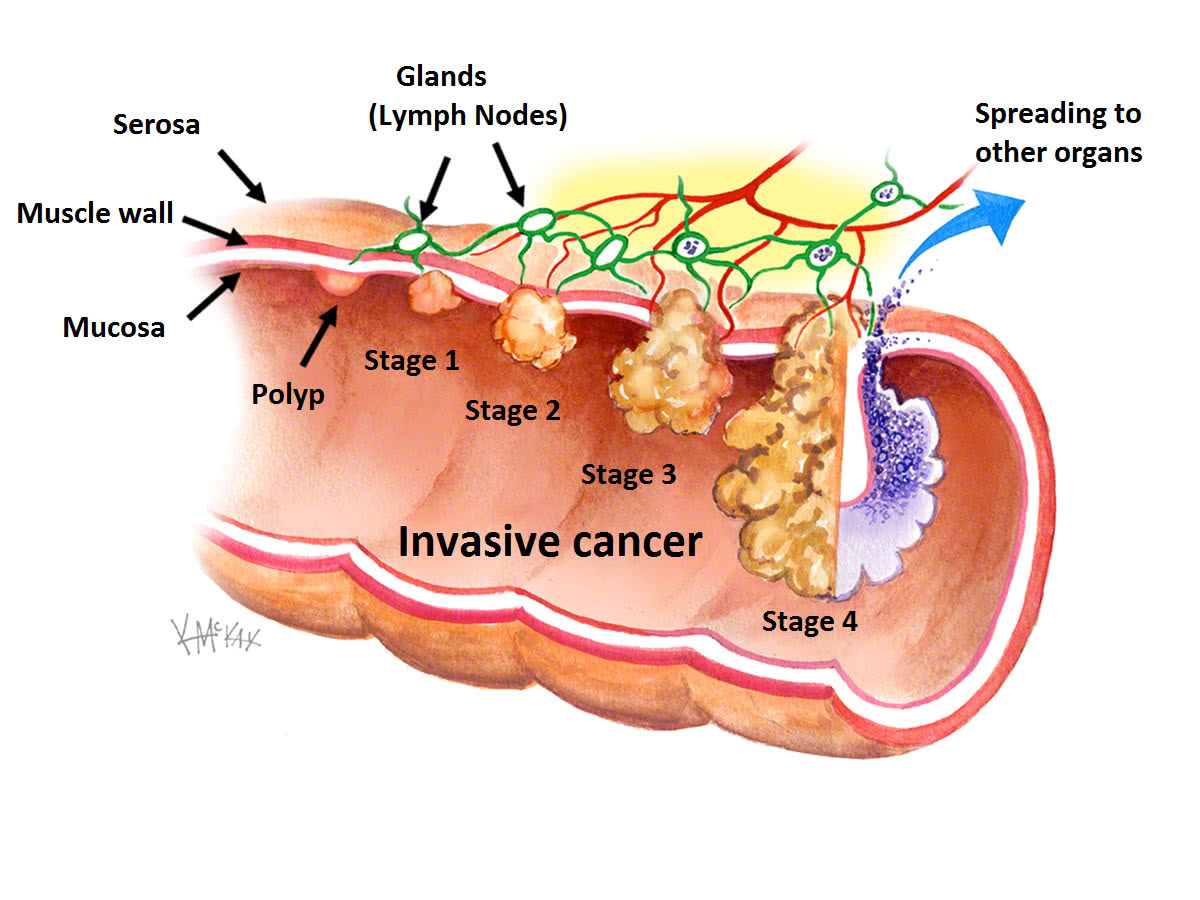
Colorectal cancer is the second largest cancer cause of death in Australia. Polyps are precursor lesions than can become cancer if not removed (Figure 5).