The following factors put you at increased risk for skin cancer:
- Ultraviolet (UV) light exposure: Extensive lifetime sun exposure or occasional intense exposure causing a sunburn
- Tanning bed use
- Age: The longer you are exposed to the sun over time, the higher your risk of developing skin cancer
- Having a fair complexion, blonde or red hair, freckles, blue eyes and/or a tendency to sunburn
- Having 50 or more moles
- There are also skin cancer risk factors linked to your personal and family medical history:
A personal or family history of skin cancer, including melanoma
- Immunosuppression, typically due to taking immunosuppressive drugs
- Previous serious skin injuries, such as a major scar or burn
- History of actinic (solar) keratoses. These are precancerous lesions.
- Familial Atypical Multiple Mole Melanoma Syndrome (FAMMMS)
- Certain rare genetic disorders, including xeroderma pigmentosum and basal cell nevus syndrome
What to expect at your skin screening exam
During a skin cancer screening exam, your doctor will look all over your body for signs of actinic keratoses (precancers), basal cell and squamous cell carcinomas. They also will look for abnormal moles that can signal melanoma.
If your dermatologist finds a suspicious mole or growth, they will determine whether it’s best to monitor it or remove it. They may take photos to aid in monitoring the lesions.
If the mole or growth is suspicious, your doctor may recommend a skin biopsy. A biopsy will remove a part or all of the growth so that it can be sent for evaluation by a pathologist. You should get the results within a week, along with follow-up instructions from your doctor.
Dermatologists are highly skilled at recognizing problem areas on your skin. But if you have noticed any changes or have any concerning areas, be sure to point them out.
How to spot skin cancer
Whether or not you are at increased risk for skin cancer, you should be familiar with your skin and be on the lookout for spots, sores that don't heal and abnormal or changing moles. Report them to your doctor without delay.
Look for new spots or spots that change.
Watch for sores that don’t heal or heal then return.
Be aware of spots or sores that change in sensation or are itchy, tender or painful.
Check everywhere. Skin cancer can develop in places that do not get sun exposure. This includes under your arms, the soles of your feet, buttocks and genital areas.
Get help to inspect hard-to-see areas such as the scalp.
Look for areas of concern when you shampoo, shower or apply lotion.
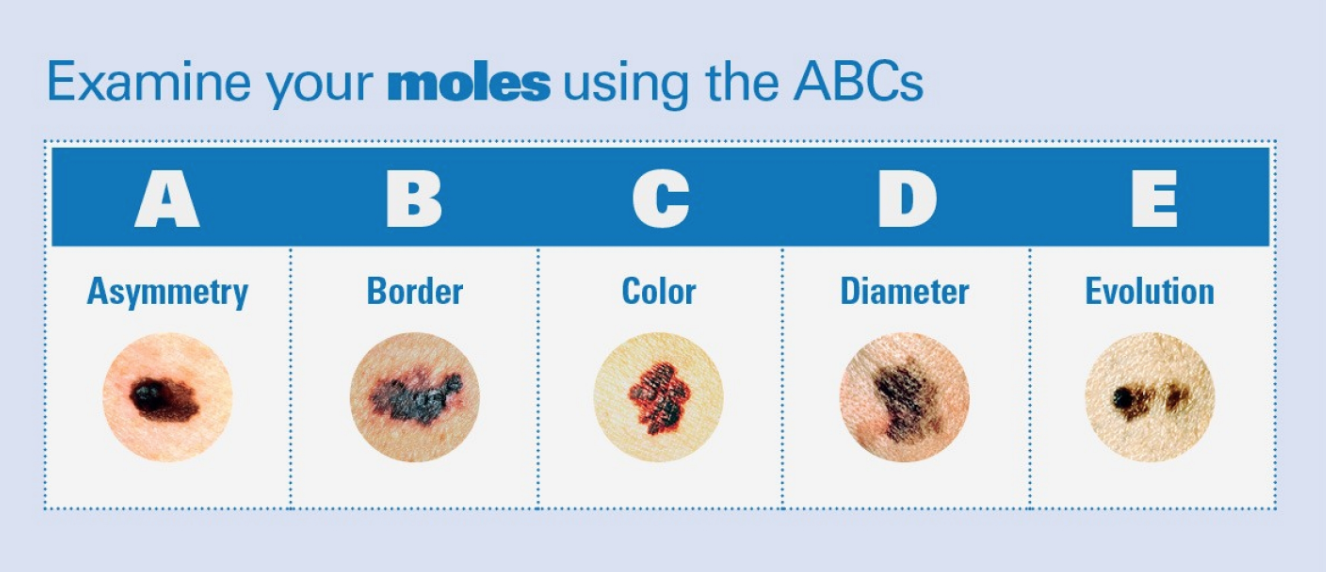
Melanomas are often asymmetrical. That means the two sides look different from each other. They often have borders that are blurry, scalloped or jagged. Melanomas also often have many colors or are haphazardly colored. You should also look at the size. A mole that is larger than 6 millimeters, or the size of a pencil eraser, is cause for concern.
Talk with your doctor if you notice any of the ABCDEs of melanoma, or if you have a mole that is evolving or changing in size, shape or feeling.

Suspicious spots or unusual moles can be a sign of skin cancer. Talk to your doctor if you are concerned.
Exams for those who have had melanoma
If you’ve had melanoma (a type of skin cancer), you need a different plan to check for cancer recurrence.
The screening plans on this page apply to people expected to live for at least 10 years. They’re not for people who have a health condition that may make it hard to diagnose or treat skin cancer. Your doctor can help you decide if you should continue screening after age 75.













