Skin Cancer (Non-Melanoma) - Introduction
ON THIS PAGE: You will find some basic information about this disease and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Non-Melanoma Skin Cancer. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
About the skin
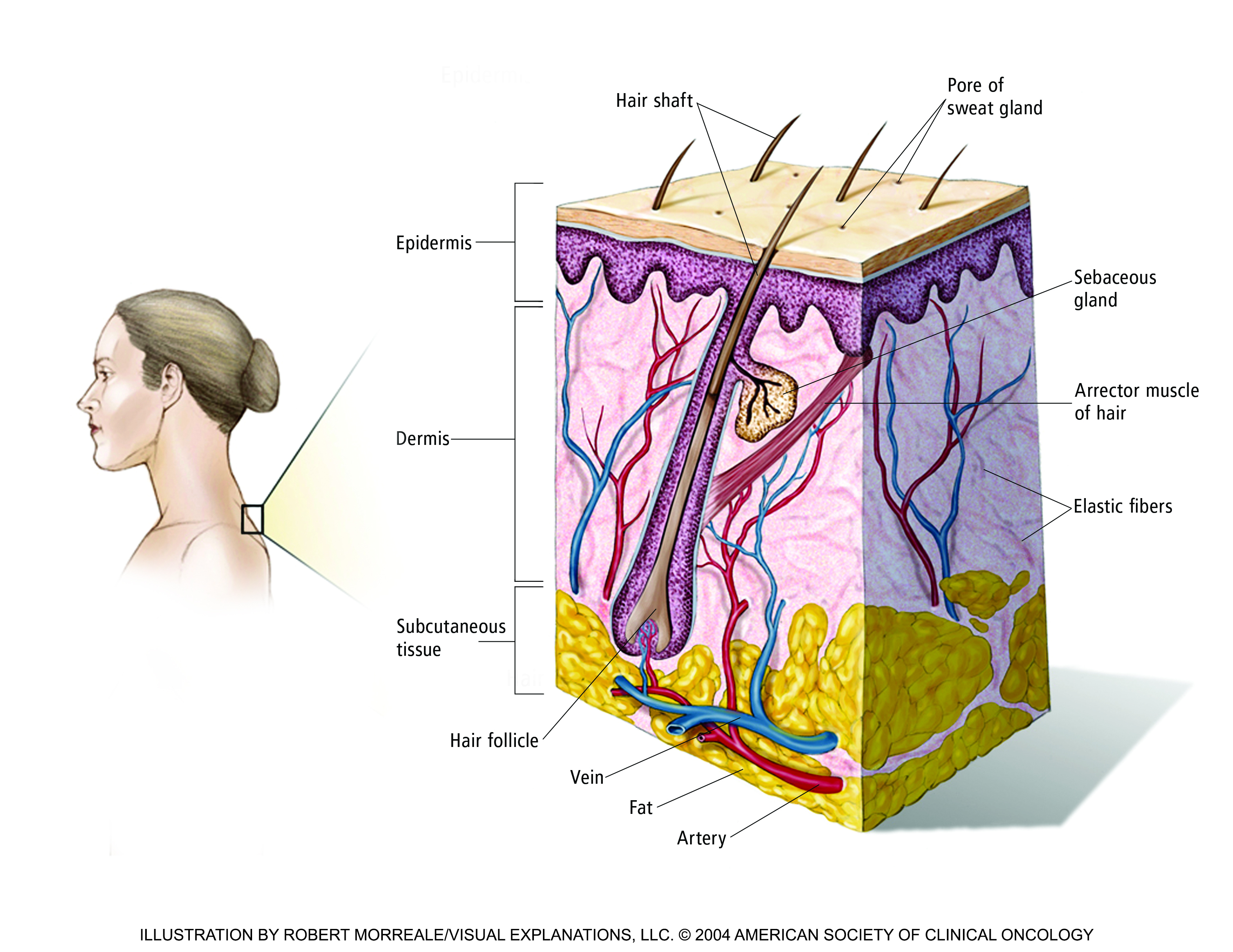
The skin is the body’s largest organ. It protects the body against infection and injury and helps regulate body temperature. The skin also stores water and fat and produces vitamin D.
The skin is made up of 3 main layers:
-
The epidermis. The outer layer of skin.
-
The dermis. The inner layer of skin.
-
The hypodermis. The deep layer of fat.
See the Medical Illustrations section for a drawing of these layers.
About skin cancer
Cancer begins when healthy cells change and grow out of control, forming a mass called a tumor. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but will not spread.
Doctors diagnose skin cancer in more than 3 million Americans each year, making it the most common type of cancer. If skin cancer is found early, it can usually be treated with topical medications, procedures done in the office by a dermatologist, or an outpatient surgery. A dermatologist is a doctor who specializes in diseases and conditions of the skin. As a result, skin cancer is responsible for less than 1% of all cancer deaths.
In some cases, skin cancer may be more advanced and require management by a multidisciplinary team that often includes a dermatologist, surgical oncologist, radiation oncologist, and a medical oncologist. These doctors will meet with a patient, and together they will recommend the best path forward to treat the cancer. In some instances, the surgical oncologist will recommend a surgery to be performed in an operating room when the procedure to treat the cancer is too extensive for an office setting. Other times, radiation therapy and/or treatments using medication given by mouth or by vein are recommended by the team either in place of or in combination with surgery. (More details are given in the Types of Treatment section of this guide.)
Types of skin cancer
There are 4 main types of skin cancer:
-
Basal cell carcinoma. Basal cells are the round cells found in the lower epidermis. About 80% of skin cancers develop from this type of cell. These cancers are described as basal cell carcinomas. Basal cell carcinoma most often develops on the head and neck, although it can be found anywhere on the skin. It is mainly caused by sun exposure or develops in people who received radiation therapy as children. This type of skin cancer usually grows slowly and rarely spreads to other parts of the body.
-
Squamous cell carcinoma. Most of the epidermis is made up of flat, scale-like cells called squamous cells. Around 20% of skin cancers develop from these cells, and these cancers are called squamous cell carcinomas. Squamous cell carcinoma is mainly caused by sun exposure, so it may be diagnosed on many regions of the skin. It can also develop on skin that has been burned, damaged by chemicals, or exposed to x-rays. Squamous cell carcinoma is commonly found on the lips; at sites of a long-standing scar; and on the skin outside the mouth, anus, and vagina. About 2% to 5% of squamous cell carcinomas spread to other parts of the body.
-
Merkel cell cancer. Merkel cell cancer is a highly aggressive, or fast-growing, rare cancer. It starts in hormone-producing cells just beneath the skin and in the hair follicles. It is usually found in the head and neck region. Merkel cell cancer may also be called neuroendocrine carcinoma of the skin. Learn more about neuroendocrine tumors.
-
Melanoma. There are scattered cells called melanocytes where the epidermis meets the dermis. These cells produce the pigment melanin, which gives skin its color. Melanoma starts in melanocytes, and it is the most aggressive type of skin cancer. It accounts for about 1% of all skin cancers. For more information about melanoma, visit the melanoma section on this same website.
Basal cell carcinoma and squamous cell carcinoma are sometimes grouped together and called keratinocyte carcinoma. This is because they begin in a type of skin cell called a keratinocyte. In this guide, "non-melanoma skin cancer" refers to keratinocyte carcinoma and Merkel cell cancer to distinguish them from melanoma.
There are a few other, rare types of non-melanoma skin cancer not covered in this guide, including cutaneous (skin) lymphomas , Kaposi sarcoma , skin adnexal tumors, and sarcomas .
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
ASCO Answers
Fact Sheet:
Read a 1-page fact sheet
that offers an introduction to squamous cell carcinoma. This free fact sheet is available as a PDF, so it is easy to print.
- Cancer.Net En Español: Read about skin cancer in Spanish. Infórmase sobre cáncer de piel no melanomatoso en español.
The next section in this guide is Statistics . It helps explain the number of people who are diagnosed with non-melanoma skin cancer and general survival rates. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Statistics
ON THIS PAGE: You will find information about the estimated number of people who will be diagnosed with non-melanoma skin cancer each year. You will read also general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with cancer are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this cancer and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for you individually. The original sources for these statistics are provided at the bottom of this page.
How many people are diagnosed with non-melanoma skin cancer?
Skin cancer is the most common type of cancer in the United States. Because non-melanoma skin cancer/keratinocyte carcinoma is so common and most often curable, statistics are estimated. This is because individual cases are not usually reported to cancer registries.
In 2012, it was estimated that 5.4 million cases of basal cell carcinoma and squamous cell carcinoma were diagnosed in the United States among 3.3 million people. Some people are diagnosed with more than 1 skin cancer. The number of non-melanoma skin cancers has been growing for several years. This is likely due to earlier detection of the disease, increased sun exposure, and longer life spans. Basal cell carcinoma is far more common than squamous cell carcinoma. About 80% of non-melanoma skin cancers are basal cell carcinoma.
In the United States, the rate of non-melanoma skin cancer deaths from these skin cancers have been declining in recent years. It is estimated that about 2,000 people die from basal cell and squamous cell skin cancer each year. Older adults and people with a suppressed immune system have a higher risk of dying from these types of skin cancer. It is estimated that 7,990 people will die from melanoma in the United States in 2023. For other, less common types of skin cancer, 4,480 people are estimated to die in 2023.
Approximately 2,000 people in the United States are diagnosed with Merkel cell cancer each year. This number has been rising rapidly the last few decades. A significant majority of people diagnosed with the disease are older than 70, and 90% of Merkel cell cancer diagnoses occur in White people. Percent means how many out of 100. Men are twice as likely to be diagnosed with the disease than women.
What is the survival rate for non-melanoma skin cancer?
There are different types of statistics that can help doctors evaluate a person’s chance of recovery from non-melanoma skin cancer. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having cancer may affect life expectancy. Relative survival rate looks at how likely people with non-melanoma skin cancer are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this cancer.
Example: Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) will be alive in 5 years.
It is important to remember that statistics on the survival rates for people with non-melanoma skin cancer are only an estimate. They cannot tell an individual person if cancer will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
Because non-melanoma skin cancer can often be cured, there is very little information on survival rates for basal cell carcinoma and squamous cell carcinoma.
The 5-year relative survival rate for Merkel cell cancer is 65%.
The survival rates for Merkel cell cancer vary based on several factors. These include the stage of cancer, a person’s age and general health, and how well the treatment plan works.
If Merkel cell cancer is found early, before it has spread from where it started, the 5-year relative survival rate is 75%. If the cancer has spread to nearby tissues or organs and/or the regional lymph nodes, the 5-year relative survival rate is 61%. Lymph nodes are small, bean-shaped organs that help fight infection. If the cancer has spread to other, distant parts of the body, the 5-year relative survival rate is 24%.
Experts measure relative survival rate statistics for non-melanoma skin cancer every 5 years. This means the estimate may not reflect the results of advancements in how non-melanoma skin cancer is diagnosed or treated from the last 5 years. Talk with your doctor if you have any questions about this information. Learn more about understanding statistics .
Statistics adapted from the American Cancer Society's (ACS) publication, Cancer Facts & Figures 2023, the ACS website, and the International Agency for Research on Cancer website. (All sources accessed March 2023.)
The next section in this guide is Medical Illustrations . It offers a drawing of the structures and layers that make up the skin. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Medical Illustrations
ON THIS PAGE: You will find a basic drawing of the structures and layers that make up the skin. Use the menu to see other pages.
See pictures of the features of basal cell carcinoma and of the signs of squamous cell carcinoma . (Please note that these links will take you to a different website.)
The next section in this guide is Risk Factors and Prevention . It describes the factors that may increase the chance of developing non-melanoma skin cancer. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Risk Factors and Prevention
ON THIS PAGE: You will find out more about the factors that increase the chance of developing non-melanoma skin cancer. Use the menu to see other pages.
A risk factor is anything that increases a person’s chance of developing cancer. Although risk factors can influence the development of cancer, most do not directly cause cancer. Some people with several risk factors never develop cancer, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor may help you make more informed lifestyle and health care choices.
The following factors may raise a person’s risk of developing non-melanoma skin cancer:
-
Sun exposure. Exposure to ultraviolet (UV) radiation from the sun plays a major role in the development of skin cancer. People who live at high altitudes or in areas with bright sunlight year-round have a higher risk of developing skin cancer. People who spend a lot of time outside during the midday hours also have a higher risk. Recreational suntanning should be avoided to reduce the risk of skin cancer.
Exposure to ultraviolet type B (UVB) radiation appears to be more closely linked with skin cancer, but ultraviolet type A (UVA) may also play a role in the development of basal cell carcinoma, squamous cell carcinoma, and melanoma . UVB radiation causes sunburn and does not penetrate car windows or other types of glass. However, UVA can pass through glass and may cause aging and wrinkling of the skin in addition to skin cancer. Therefore, it is important to protect your skin from both UVA and UVB radiation (see “Prevention,” below).
Because Merkel cell cancer often occurs on the sun-exposed areas of the head and neck, many doctors think that sun exposure may also be a risk factor for this type of cancer.
-
Weakened or suppressed immune system. People with a weakened immune system due to a bone marrow/stem cell transplant, organ transplant, or a disease such as human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) or certain types of leukemia have a higher risk of developing skin cancer, particularly squamous cell carcinoma. People taking immunosuppressive drugs have the same higher risk.
-
Indoor tanning. People who previously have used or actively use tanning beds, tanning parlors, or sun lamps have an increased risk of developing all types of skin cancer. There is no safe amount of indoor tanning. Any use of indoor tanning devices increases the risk of skin cancer, including melanoma, and this risk increases with more use of indoor tanning.
-
Fair skin/complexion. People with lighter colored skin, blond or red hair, blue eyes, and freckles are at increased risk for developing skin cancer. People whose skin has a tendency to burn rather than tan also have an increased risk. However, all people, regardless of skin color, are at risk for developing skin cancer.
-
Race/ethnicity. Lighter-skinned people are more likely to develop basal cell carcinoma, squamous cell carcinoma, Merkel cell cancer, and melanoma. However, darker-skinned people can still develop the disease.
-
Precancerous skin conditions. Rough, red, or brown scaly patches on the skin, called actinic keratoses or Bowen's disease, are usually more common in areas exposed to the sun. These areas can change into squamous cell cancers in a small number of people. The more actinic keratoses a person has, the higher the risk that they will develop a squamous cell carcinoma. Using a broad-spectrum sunscreen throughout the year that protects against both UVA and UVB radiation and has a sun protection factor (SPF) of 30 or more helps decrease the risk of developing actinic keratoses. See the "Prevention" section below for more information about protecting your skin from the sun.
-
Gender. The number of older White men and younger White women who have developed skin cancer in recent years has increased. Also, in general, men are more likely to develop Merkel cell cancer.
-
Age. Most basal cell and squamous cell carcinomas typically appear after age 50. However, in recent years, the number of skin cancers in people age 65 and older has increased dramatically. This may be due in part to better screening and patient tracking efforts in skin cancer. Younger people can also develop non-melanoma skin cancer, especially if they have lighter skin, an inherited (genetic) syndrome that puts them at high risk (see below), or been exposed to significant amounts of radiation or UV radiation from the sun. Merkel cell cancer is most common in people older than age 70.
-
A history of sunburns or fragile skin. Skin that has been burned, sunburned, or injured from disease has a higher risk of skin cancer. Squamous cell and basal cell carcinoma occur more often in people who have more exposure to the sun or other sources of UV radiation over their lifetime.
-
Previous skin cancer. People who have had any form of skin cancer have a higher risk of developing another skin cancer. From 35% to 50% of people diagnosed with 1 basal cell carcinoma will develop a new skin cancer within 5 years. Therefore, people who have had 1 skin cancer need ongoing follow-up care to watch for additional cancers. See the Follow-up Care section for more information.
-
Inherited syndromes. Certain rare genetic conditions are associated with an increased risk of developing basal cell carcinoma. These conditions include nevoid basal cell carcinoma syndrome , which is also called Gorlin syndrome, and the very rare Rombo, Bazex-Dupré-Christol, and epidermolysis bullosa simplex syndromes, among others. Rare syndromes associated with an increased risk of squamous cell carcinoma include xeroderma pigmentosum , albinism, epidermolysis bullosa simplex, dyskeratosis congenita, and multiple self-healing squamous epitheliomata.
-
Medications. In addition to medications that suppress the immune system, certain steroids and medications that make the skin very sensitive to sunburns have all been shown to increase a person’s risk of developing squamous cell carcinoma. Examples include vandetanib (Caprelsa), vemurafenib (Zelboraf), and voriconazole (Vfend). Certain BRAF inhibitor targeted therapies, including dabrafenib (Tafinlar), encorafenib (Braftovi), and vemurafenib, have been shown to increase a person’s risk of developing squamous cell carcinoma by turning on a growth pathway in cells that tend to turn into this type of cancer (for example, cells with an HRAS mutation).
-
Previous treatment with radiation therapy. When a person receives radiation therapy to treat cancer, they have a higher risk of developing basal cell carcinoma. This risk increases over time, especially after 10 to 20 years. As a result, children who receive radiation therapy have a 6 times higher risk for developing a basal cell carcinoma.
-
Human papillomavirus (HPV). Research shows that the HPV virus is a risk factor for squamous cell carcinoma, particularly if the person’s immune system becomes suppressed. Sexual activity with someone who has HPV is the most common way someone gets HPV. There are different types of HPV, called strains. Research links some HPV strains more strongly with certain types of cancers. HPV vaccines can prevent people from developing certain cancers. Learn more about HPV and cancer.
-
Merkel cell polyomavirus (MCV). Research indicates that there is a link between this virus and Merkel cell cancer. MCV is present in up to an estimated 80% of Merkel cell cancers. However, scientists believe MCV is common, while Merkel cell cancer is not. More research is needed to learn the role of MCV in this connection.
-
Arsenic exposure. Exposure to the poison arsenic may increase the risk of Merkel cell cancer.
Prevention
Different factors cause different types of cancer. Researchers continue to look into what factors cause non-melanoma skin cancers, including ways to prevent it. Although there is no proven way to completely prevent skin cancer, you may be able to lower your risk. Talk with your health care team for more information about your personal risk of cancer.
Reducing exposure to UV radiation, particularly by reducing time spent in the sun and avoiding indoor tanning, lowers the risk of developing skin cancer. This is important for people of all ages and is especially important for people who have other risk factors (see above). Sun damage builds up over time. The following steps can reduce sun exposure and avoid sunburn:
-
Limit or avoid direct exposure to the sun between 10:00 AM and 4:00 PM.
-
Wear sun-protective clothing, including a wide-brimmed hat that shades the face, neck, and ears. Clothes made from fabric labeled with UV protection factor (UPF) may provide better protection. UV-protective sunglasses are also recommended.
-
Use a broad-spectrum sunscreen throughout the year that protects against both UVA and UVB radiation and is SPF 30 or more. Reapply at least 1 ounce of sunscreen to your entire body every 2 hours or every hour after heavy sweating or being in the water.
-
Avoid recreational sunbathing.
-
Do not use sun lamps, tanning beds, or tanning salons.
-
Examine the skin regularly. This should include examinations by a health care professional and self-examinations. Learn more about how to do a self-examination .
-
In research, taking 500mg of nicotinamide, a form of vitamin B3, as a tablet twice daily showed a reduction in skin cancers other than melanoma by 23% in people who had 2 or more previous skin cancers. Talk with your doctor before taking any supplements.
Learn more about protecting your skin from the sun .
Limiting your sun exposure may reduce your body’s production of vitamin D, although some research suggests that most people may only need 15 minutes of sunlight exposure daily to produce enough vitamin D. People with limited sun exposure should talk with their doctor about how to include good sources of vitamin D in their diet, including the use of supplements. Your levels of vitamin D can be checked by your doctor using a simple blood test.
The next section in this guide is Screening . It describes the early warning signs of skin cancer and how to perform a self-examination. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Screening
ON THIS PAGE: You will find out more about screening for non-melanoma skin cancer and what to look for during self-examination. Use the menu to see other pages.
Screening is used to look for cancer before you have any symptoms or signs. Scientists have developed, and continue to develop, tests that can be used to screen a person for specific types of cancer before signs or symptoms appear. The overall goals of cancer screening are to:
-
Lower the number of people who die from the disease, or eliminate deaths from cancer altogether by identifying cancer at an earlier and more treatable stage
-
Lower the number of people who develop the disease
Learn more about the basics of cancer screening and what to expect during a skin cancer screening , in separate articles on this website.
Screening information for non-melanoma skin cancer
Early detection and recognition of skin cancer are very important. More than 75% of non-melanoma skin cancers are noticed first by patients or their families. Recognizing the early warning signs of skin cancer and doing regular self-examinations of your skin can help find skin cancer early, when the disease is more likely to be cured.
Self-examinations should be performed in front of a full-length mirror in a brightly lit room. It helps to have another person check the scalp and back of the neck. For people with lighter skin, non-melanoma skin cancer most often begins in places that are frequently exposed to the sun. For people with darker skin, squamous cell carcinoma often occurs in areas that are not as frequently exposed to the sun, such as the lower legs.
Include the following steps in a skin self-examination:
-
Examine the front and back of the entire body in a mirror, then the right and left sides, with arms raised.
-
Bend the elbows and look carefully at the outer and inner forearms, upper arms (especially the hard-to-see back portion), and hands.
-
Look at the front, sides, and back of the legs and feet, including the soles and the spaces between the toes.
-
Part the hair to lift it and examine the back of the neck and scalp with a hand mirror.
-
Check the back, genital area, and buttocks with a hand mirror.
Talk with your doctor if your hairdresser or barber has noticed a suspicious lesion on your scalp or under your beard, or if you find any of the following during self-examination:
-
A growth on the skin that matches the symptoms and signs of non-melanoma skin cancer
-
New growth on the skin
-
A suspicious change in an existing mole or spot
-
A sore that does not heal within 2 weeks
The next section in this guide is Symptoms and Signs . It explains what changes or medical problems non-melanoma skin cancer can cause. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Symptoms and Signs
ON THIS PAGE: You will find out more about changes and other things that can signal a problem that may need medical care. Use the menu to see other pages.
People with a basal cell carcinoma, squamous cell carcinoma, or Merkel cell cancer may experience the following symptoms or signs. Symptoms are changes that you can feel in your body. Signs are changes in something measured, like by taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. Sometimes, people with non-melanoma skin cancer do not have any of the symptoms and signs described below. Or, the cause of a symptom or sign may be a medical condition that is not cancer.
Changes in the skin are the main warning sign for skin cancer. Each type of skin cancer can appear differently, so it is important to talk with your doctor when you notice a change in your skin. The skin features that frequently develop are listed below.
For basal cell carcinoma , 2 or more of the following features may be present:
-
An open sore that bleeds, oozes, or crusts and remains open for several weeks
-
A reddish, raised patch or irritated area that may crust or itch, but rarely hurts
-
A shiny pink, red, pearly white, or translucent bump
-
A pink growth with an elevated border and crusted central indentation
-
A scar-like, white, yellow, or waxy area, often with a poorly defined border
See pictures of these features of basal cell carcinoma . (Please note that this link will take you to a separate website.)
Squamous cell carcinoma can often crust, bleed, and appear as:
-
A wart-like growth
-
A persistent, scaly red patch with irregular borders that may bleed easily
-
An open sore that persists for weeks
-
A raised growth with a rough surface and a central depression
See pictures of these signs of squamous cell carcinoma . (Please note that this link will take you to a separate website.)
Merkel cell cancer often occurs as:
-
Painless, firm, shiny lumps on the skin
-
These lumps can be red, pink, or blue
Some types of skin cancer spread along the nerves. If this happens, it can cause itching, pain, numbness, tingling, or a feeling like there are ants crawling under the skin. Other signs may include a lump or bump under the skin in areas such as the neck, armpit, or groin.
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will ask how long and how often you’ve been experiencing the symptom(s), in addition to other questions. This may include when you first noticed the skin feature, how long it has been there, and any other symptoms you may be experiencing. This is to help figure out the cause of the problem, called a diagnosis.
For most cases of skin cancer, removing the cancer with surgery or using a topical treatment will cure the disease. In more complicated cases, a multidisciplinary team of doctors will meet with a patient to discuss different types of treatments to develop a plan with the best chances of curing or controlling this disease (see Types of Treatment ).
Particularly with advanced skin cancer, relieving symptoms will be an important part of cancer care and treatment. Managing symptoms may also be called "palliative care" or "supportive care." Once started, it is continued throughout treatment. Be sure to talk with your health care team about the symptoms you experience, including any new symptoms or a change in symptoms.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Diagnosis
ON THIS PAGE: You will find a description of the common test doctors use to find out whether a suspicious mole, slow-healing sore, or other skin feature is cancerous. Use the menu to see other pages.
More than 75% of non-melanoma skin cancers are first noticed by patients or family members. That is why it is important to bring any suspicious area on your skin to a doctor’s attention. Doctors use many tests to find, or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If the cancer has spread, it is called metastasis. Doctors may also do tests to learn which treatments could work best.
How skin cancer is diagnosed
For most types of cancer, a biopsy is the only sure way for the doctor to know if an area of the body has cancer. Your doctor may consider these factors when choosing a diagnostic test:
-
The type of cancer suspected
-
Your signs and symptoms
-
Your age and general health
-
The results of earlier medical tests
Because non-melanoma skin cancer rarely spreads, a biopsy is often the only test needed to diagnose and find out the stage, or extent, of cancer . A biopsy is the removal of a small amount of tissue for examination under a microscope. During this procedure, the suspected skin lesion is removed, usually after a local anesthetic is used to numb the area. The doctor also often removes an area of healthy tissue around the lesion, which is called the margin.
The sample removed during the biopsy is then analyzed by a pathologist who determines if it is a skin cancer. A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease.
Your doctor will review the results of the biopsy with you. No further treatment beyond the biopsy may be necessary if the entire cancer was removed. However, if cancer cells were found in the margins of the removed tissue, additional treatment will usually be recommended. See more in the Types of Treatment section of this guide.
Learn more about how a biopsy is used to make a diagnosis .
The next section in this guide is Stages . It explains the system doctors use to describe the extent of the skin cancer. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Stages
ON THIS PAGE: You will learn about how doctors describe a cancer’s growth or spread. This is called the stage. Use the menu to see other pages.
What is cancer staging?
Staging is a way of describing where the cancer is located, if or where it has spread, and whether it is affecting other parts of the body.
Doctors use diagnostic tests to find out the cancer's stage, so staging may not be complete until all the tests are finished. Knowing the stage helps the doctor recommend the best kind of treatment, and it can help predict a patient's prognosis, which is the chance of recovery.
This page provides information about how doctors find the stage of skin cancer and the stage groups for Merkel cell cancer, such as stage II or stage IV.
-
Staging for basal cell and squamous cell carcinoma
-
Staging for Merkel cell cancer
Staging for basal cell and squamous cell carcinoma
There is no staging system for basal cell and squamous cell carcinoma because they are so often curable and usually do not spread to other parts of the body. On rare occasions, a person’s lymph node(s) may be removed to find out if the cancer has spread, which is called metastasis. Lymph nodes are bean-shaped organs that help fight infection. The doctor may recommend other tests to determine the extent of the disease, including blood tests, chest x-rays, and imaging scans of the lymph nodes and nerves, liver, bones, and brain, but this is uncommon.
Return to top
Staging for Merkel cell cancer
Doctors use the TNM system to describe the stage of Merkel cell cancer. Doctors use the results from diagnostic tests and scans to answer these questions:
-
Tumor (T): How large is the primary tumor? Where is it located?
-
Node (N): Has the tumor spread to the lymph nodes? If so, where and how many?
-
Metastasis (M): Has the cancer spread to other parts of the body? If so, where and how much?
The results are combined to determine the stage of Merkel cell cancer for each person.
There are 5 stages: stage 0 (zero) and stages I through IV (1 through 4). The stage provides a common way of describing the cancer, so doctors can work together to plan the best treatments.
Stage 0: This is called carcinoma in situ or a precancerous lesion. Cancer cells are found only in the top layers of the skin.
Stage I: The primary tumor is 2 centimeters (cm) or smaller at its widest part. The cancer has not spread to the lymph nodes or to other parts of the body.
Stage IIA: The tumor is larger than 2 cm and has not spread to the lymph nodes or other parts of the body.
Stage IIB: The tumor has grown into nearby tissues, such as muscles, cartilage, or bone. It has not spread to the lymph nodes or elsewhere in the body.
Stage III: The cancer has spread to the lymph nodes. The tumor can be any size and may have spread to nearby bone, muscle, connective tissue, or cartilage.
-
Stage IIIA: The tumor is any size or may have grown into nearby tissues. Biopsy or surgery has found that the cancer has spread to nearby lymph nodes. The cancer has not spread to other parts of the body. Or, there is no sign of a tumor, but cancer was found in a nearby lymph node during an exam or with imaging scans. Its presence was confirmed using a microscope.
-
Stage IIIB: The tumor is any size or may have grown into nearby tissues. The cancer has spread through the lymphatic system, either to a regional lymph node located near where the cancer started or to a skin site on the way to a lymph node, called “in-transit metastasis.” In-transit metastasis may have reached these other lymph nodes. The lymphatic system is part of the immune system and drains fluid from body tissues through a series of tubes or vessels.
Stage IV: The tumor has spread to distant parts of the body, such as the liver, lung, bone, or brain.
Used with permission of the American College of Surgeons, Chicago, Illinois. The original and primary source for this information is the AJCC Cancer Staging Manual, Eighth Edition (2017) , published by Springer International Publishing.
Return to top
Information about the cancer’s stage will help the doctor recommend a specific treatment plan. The next section in this guide is Types of Treatment . Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Types of Treatment
ON THIS PAGE: You will learn about the different types of treatments doctors use for people with non-melanoma skin cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for this type of cancer. “Standard of care” means the best treatments known. When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials are an option. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How skin cancer is treated
In cancer care, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. For non-melanoma skin cancer, these doctors may include dermatologists, surgeons or surgical oncologists, plastic surgeons, radiation oncologists, and medical oncologists. This is called a multidisciplinary team . When a multidisciplinary care team meets to discuss a case, it is often called a tumor board. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including the size and location of the skin cancer, possible side effects, and the patient’s preferences and overall health. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of talks are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is particularly important for non-melanoma skin cancer because there are different treatment options. Learn more about making treatment decisions .
The common types of treatments used for non-melanoma skin cancer are described below. Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
-
Surgery
-
Radiation therapy
-
Other local treatments
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
-
Physical, social, and emotional effects of cancer
-
Metastatic or advanced skin cancer
-
Remission and the chance of recurrence
Surgery
Surgery is the removal of the tumor and surrounding tissue during a medical procedure. Many skin cancers can be removed from the skin quickly and easily during a simple surgical procedure. Often, no other treatment is needed.
Which surgical procedure is used depends on the type of skin cancer and the size and location of the lesion. Most of these procedures use a local anesthetic to numb the skin first. They can be done by a dermatologist, surgical oncologist, general surgeon, plastic surgeon, nurse practitioner, or physician assistant in their clinic setting, outside of a hospital. Other procedures, such as more extensive wide excisions and sentinel lymph node biopsies, are performed in a hospital operating room with local and/or general anesthesia. This is often done for Merkel cell cancer.
Surgeries and other procedures for non-melanoma skin cancer include:
-
Curettage and electrodesiccation. During this common procedure, the skin lesion is removed with a curette, which is a sharp, spoon-shaped instrument. The area is then treated with an electric current that helps control bleeding and destroys any remaining cancer cells. This is called electrodesiccation. Many people have a flat scar after healing from this procedure.
-
Mohs micrographic surgery. This technique, also known as complete margin assessment surgery, involves removing the visible tumor in addition to small fragments around the edge of the area where the tumor was located. Each small fragment is examined under a microscope until all of the cancer is removed. This is typically used for larger tumors, for those located in the head and neck region, and for cancers that have come back in the same place.
-
Wide excision. This involves the removal of the tumor and some surrounding healthy skin and soft tissue, called a margin. How much tissue is removed depends on the type and size of the skin cancer. When a large tumor is removed, the incision may be too large to close, so surgeons may use skin from another part of the body to close the wound. This is called a skin graft.
-
Reconstructive surgery. Since skin cancer often develops on a person’s face, a reconstructive (plastic) surgeon may be part of the health care team. When doctors plan treatment, they consider how treatment might affect a person’s quality of life, such as how the person feels, looks, talks, and eats. Before any surgery for skin cancer, talk with your doctor about whether changes to your appearance are possible and whether there may be functional aspects that need to be considered when developing a treatment plan.
-
Sentinel lymph node biopsy. This surgical procedure, also called SLNB, sentinel node biopsy, or SNB, is often used for Merkel cell cancer. It helps the doctor find out whether the cancer has spread to the lymph nodes. When cancer spreads from the place it started to the lymph nodes, it travels through the lymphatic system. A sentinel lymph node is the first lymph node into which the lymphatic system drains from the initial tumor site. Because cancer can start anywhere on the skin, the location of the sentinel lymph nodes will be different for each patient, depending on where the cancer started. To find the sentinel lymph node, a dye and a harmless radioactive substance is injected as close as possible to where the cancer started. The substance is followed to the sentinel lymph node. Then, the doctor removes 1 or more of these lymph nodes to check for cancer cells, leaving behind most of the other lymph nodes in that area. These are sent to a pathologist who analyzes the lymph nodes and then provides a report. If cancer cells are not found in the sentinel lymph node(s), no further lymph node surgery is needed. If the sentinel lymph node contains cancer cells, this is called a positive sentinel lymph node. This means the disease has spread, and further treatment, including additional surgery, may be recommended.
Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have. In general, surgery may include side effects such as pain, scarring, numbness, skin stretching, wound problems, infection, and changes in appearance where the surgery was performed. Learn more about the basics of cancer surgery .
Return to top
Radiation therapy
Radiation therapy is the use of high-energy rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. Radiation therapy may be used instead of surgery for skin cancer that is located in a hard-to-treat place, such as on the eyelid , the tip of the nose, or the ear. It is also used in some people who would like to avoid scarring from surgery. Finally, radiation therapy may be recommended after surgery, especially for lymph nodes that are involved in the cancer, to help prevent the skin cancer from coming back.
For Merkel cell cancer, radiation therapy is often given after surgery for stage I and II disease. This is called adjuvant therapy.
The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. Several treatments may be needed to eliminate the cancer. A less common type of radiation treatment for skin cancer is brachytherapy. This involves placing the radiation source very close to or inside of the skin cancer.
Radiation therapy is not recommended for people with nevoid basal cell carcinoma syndrome .
The side effects from radiation therapy may include a rash, skin infections, itchy or inflamed skin, or a change in the color of the skin. However, these side effects can usually be prevented by applying a corticosteroid or antibiotic to the skin. If side effects develop, most go away a few weeks after treatment has finished. Learn more about the basics of radiation therapy .
Return to top
Other local treatments
To treat precancerous skin conditions or a cancerous lesion located only in the top layer of the skin, doctors may use photodynamic therapy, cryotherapy, or laser therapy.
Photodynamic therapy. This is a combination treatment for actinic keratoses (see Risk Factors and Prevention ). First, a topical medication called aminolevulinic acid (Levulan) is applied over areas with many actinic keratoses. Then this area is exposed to a special light-emitting device for several minutes to a few hours. The aminolevulinic acid makes the skin very sensitive, so the procedure can be painful. Your doctor may recommend taking pain medication before the procedure. In addition, the chemical makes the skin very sensitive to the sun, so it is important to avoid sun exposure and wear protective glasses, clothing, and sunscreen for a few days after the procedure. The skin will remain very irritated for a few days, but the actinic keratoses quickly disappear once the irritation goes away.
Freezing. This procedure, which is also called cryotherapy, uses liquid nitrogen to freeze and destroy abnormal cells. It is usually used to treat precancerous skin conditions. The liquid nitrogen will sting when it is first applied to the skin, and then the skin will blister and shed off. More than 1 freezing may be needed. Sometimes this procedure leaves a scar.
Laser therapy. A narrow beam of high-intensity light can destroy precancerous skin conditions that are located only in the outer layer of the skin.
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication. For some skin cancers, these medications may also be prescribed by a dermatologist.
Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for non-melanoma skin cancer include:
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
Each of these types of therapies is discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications.
It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases .
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. In skin cancer treatment, these drugs are usually applied to the skin every day for several weeks. This is called topical treatment. These types of medications may cause the side effects of skin inflammation or irritation, which generally go away after treatment is finished.
Topical diclofenac (Solaraze), fluorouracil (multiple brand names), and ingenol mebutate (Picato) are approved for the treatment of precancerous actinic keratoses, with fluorouracil resulting in better results in terms of effectiveness and time until new precancers appear. All of these creams can cause irritation, burning, redness, and stinging during treatment. These symptoms usually go away soon after treatment has been completed. These creams do not cause scars, which is why many doctors use them to treat the face or other areas where a person's appearance may be affected.
For small basal cell cancers not located on the face, topical imiquimod (Aldara, Zyclara), which stimulates the immune system, may be recommended. The cream must be applied once a day, 5 days a week, for 6 to 12 weeks. Topical fluorouracil is also approved by the U.S. Food and Drug Administration (FDA) to treat very thin basal cell carcinomas. It should be applied 2 times a day for 3 to 6 weeks. Some irritation and redness in the area of the basal cell carcinoma is expected with this treatment.
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all cancers have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in the cancer cells. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments .
For large (also called advanced) basal cell cancers that cannot be treated with surgery or radiation therapy, there are 2 targeted drugs, vismodegib (Erivedge) and sonidegib (Odomzo), which are FDA-approved drugs known as hedgehog pathway inhibitors. They block the PTCH1 genetic mutation, which seems to drive the growth of basal cell carcinoma. This treatment shrinks or stabilizes tumors in many patients. The main side effects of this treatment include hair thinning, muscle cramps, weight loss, dry skin, and loss of taste.
Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Return to top
Immunotherapy ( updated 04/2023 )
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system's ability to attack cancer cells.
There are 3 FDA-approved immunotherapy drugs for non-melanoma skin cancer.
-
Cemiplimab (Libtayo). This immune checkpoint inhibitor targets the PD-1 pathway. It is approved to treat metastatic or locally advanced squamous cell carcinoma and metastatic or locally advanced basal cell carcinoma.
-
Pembrolizumab (Keytruda). This is another immune checkpoint inhibitor that targets PD-1. It can be used to treat Merkel cell cancer that has spread or come back after treatment. Pembrolizumab can also be used to treat squamous cell carcinoma that is locally advanced, has spread, or has come back after treatment and cannot be treated with surgery or radiation therapy.
-
Avelumab (Bavencio). Avelumab blocks the PD-L1 pathway. It can be used to treat people 12 and older with Merkel cell cancer that has spread to another part of the body.
-
Retifanlimab (Zynyz). Retifanlimab is also a PD-1 inhibitor. It may be used to treat adults with Merkel cell cancer that has spread or has come back after treatment.
Different types of immunotherapy can cause different side effects. The common side effects of cemiplimab and pembrolizumab include fatigue, pain, decreased appetite, itching, diarrhea, nausea, rash, fever, cough, shortness of breath, and constipation. The common side effects of avelumab include fatigue, pain, diarrhea, nausea, rash, appetite loss, and swelling due to fluid buildup. Immunotherapy sometimes results in the immune system attacking healthy cells, which can also cause side effects. Talk with your doctor about possible side effects for the immunotherapy recommended for you. Learn more about the basics of immunotherapy .
Return to top
Physical, emotional, and social effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Return to top
Metastatic or advanced skin cancer
It is uncommon, but non-melanoma skin cancer can spread to another part in the body from where it started. In these situations, doctors call it metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
Surgery alone cannot always eliminate skin cancer that has metastasized. If cancer cannot be removed with surgery, it is called unresectable. To control distant spread, a person’s treatment plan may include chemotherapy, radiation therapy, and/or targeted therapy. Palliative care will also be important to help relieve symptoms and side effects.
Squamous cell carcinoma. Metastatic or unresectable squamous cell carcinoma of the skin is rare, so treatment plans often use the same treatments that have worked in people with squamous cell carcinoma of the head and neck that may not have started on the skin. Chemotherapy usually includes taxanes, such as docetaxel (Taxotere) or paclitaxel (available as a generic drug), and platinums, such as carboplatin or cisplatin (both available as generic drugs). The main side effects of these medicines include fatigue, low blood cell counts, rashes, diarrhea, and changes in sensation in the tips of the fingers or toes. Learn more about the basics of chemotherapy .
Similar to chemotherapy regimens, several targeted therapies may be used for some people with squamous cell carcinoma, also based on data from patients with squamous cell cancer of the head and neck. These include cetuximab (Erbitux), panitumumab (Vectibix), and erlotinib (Tarceva). None have been approved by the FDA for squamous cell cancer of the skin.
The use of immunotherapy to treat people with metastatic and unresectable squamous cell carcinoma has become the standard treatment approach. The PD-1 blocking drugs cemiplimab and pembrolizumab can be used to treat this diagnosis.
Basal cell carcinoma. If metastatic basal cell carcinoma cannot be treated with surgery or radiation therapy, targeted therapy may be an option. Vismodegib and sonidegib are FDA-approved drugs known as hedgehog pathway inhibitors. As described in "Targeted therapy" above, these drugs block the PTCH1 genetic mutation.
Merkel cell cancer. Treatment for metastatic Merkel cell cancer usually involves immunotherapy with avelumab or pembrolizumab (see "Immunotherapy," above). Other immunotherapy medications may be available through clinical trials. Chemotherapy, surgery, and/or radiation therapy may be used to relieve symptoms and side effects.
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning and the role of follow-up care in finding any recurrence early. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence .
If skin cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence). Certain parts of the body, such as the ears and lips, are more prone to develop recurrent skin cancers. In addition, people whose immune system is suppressed due to a medication or disease are also at higher risk for skin cancer recurrence.
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above. Your doctor may suggest clinical trials that are studying new ways to treat recurrent skin cancer. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
People with recurrent skin cancer sometimes experience fear, disbelief, and other emotions. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence .
Return to top
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - About Clinical Trials
ON THIS PAGE: You will learn more about clinical trials, which are the main way that new medical approaches are studied to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to care for people with non-melanoma skin cancer. To make scientific advances, doctors create research studies involving volunteers, called clinical trials. Every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials.
Clinical trials are used for all types and stages of non-melanoma skin cancer. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of treatments, new approaches to radiation therapy or surgery, and new methods of treatment.
People who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and the chance that the new treatment may not work. People are encouraged to talk with their health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment. Talk with your doctor about clinical trials for symptoms and side effects.
Deciding to join a clinical trial
People decide to participate in clinical trials for many reasons. For some, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the added uncertainty of a clinical trial in the hope of a better result. Others volunteer for clinical trials because they know that these studies are a way to contribute to the progress in treating skin cancer. Even if they do not benefit directly from the clinical trial, their participation may benefit future people with skin cancer.
Insurance coverage and the costs of clinical trials differ by location and by study. In some programs, some of the expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team and your insurance company first to learn if and how your treatment in a clinical trial will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, they may receive no treatment by being given a placebo or a “sugar pill.” When used, placebos are usually combined with standard treatment in most cancer clinical trials. Study participants will always be told when a placebo is used in a study. Find out more about placebos in cancer clinical trials .
Patient safety and informed consent
To join a clinical trial, people must participate in a process known as informed consent. During informed consent, the doctor should:
-
Describe all of the treatment options so that the person understands how the new treatment differs from the standard treatment.
-
List risks of the new treatment, which may or may not be different from the risks of standard treatment.
-
Explain what will be required of each person in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
-
Describe the purposes of the clinical trial and what researchers are trying to learn.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together. You will need to meet all of the eligibility criteria in order to participate in a clinical trial. Learn more about eligibility criteria in clinical trials.
People who participate in a clinical trial may stop participating at any time for personal or medical reasons. This may include that the new treatment is not working or there are serious side effects. It is important that people participating in a clinical trial talk with their doctor and researchers about who will be providing their treatment and care during the clinical trial, after the clinical trials ends, and/or if they choose to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of cancer. For specific topics being studied for non-melanoma skin cancer, learn more in the Latest Research section.
Cancer.Net offers more information about cancer clinical trials in other areas of the website, including a complete section on clinical trials and places to search for clinical trials for a specific type of cancer .
In addition, you can find a free video-based educational program about cancer clinical trials in another section of this website.
The next section in this guide is Latest Research . It explains areas of scientific research for non-melanoma skin cancer. Use the menu to choose another section to continue reading this guide.
Skin Cancer (Non-Melanoma) - Latest Research
ON THIS PAGE: You will read about the scientific research being done to learn more about non-melanoma skin cancer and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about keratinocyte carcinoma and Merkel cell cancer, ways to prevent them, how to best treat them, and how to provide the best care to people diagnosed with these diseases. The following areas of research may include new options for patients through clinical trials. Always talk with your doctor about the best diagnostic and treatment options for you.
-
EGFR inhibitors for advanced or metastatic squamous cell carcinoma. A tumor protein known as the epidermal growth factor receptor (EGFR) causes many squamous cell carcinomas to grow out of control. Several clinical trials are investigating whether combining radiation therapy with drugs that target EGFR can help treat advanced or metastatic disease.
-
Additional hedgehog pathway inhibitors for advanced basal cell carcinoma. Researchers are developing new hedgehog pathway inhibitors to treat advanced basal cell carcinoma that cannot be treated with surgery or radiation therapy.
-
Combining hedgehog pathway inhibitors with other therapies. Researchers are testing whether combining hedgehog inhibitors with other treatments, such as surgery and radiation therapy, would be helpful in treating basal cell carcinomas that are difficult to cure.
-
Immunotherapy. As outlined in Types of Treatment , immunotherapy medications are actively being studied for certain non-melanoma skin cancers, including Merkel cell cancer. These medications are usually given through a vein, and their effects can last a long time.
-
Merkel cell polyomavirus (MCV). As described in Risk Factors and Prevention , MCV is present in most but not all Merkel cell cancer tumors. Researchers continue to investigate the link between this common virus and this uncommon type of tumor, including whether the presence or absence of the virus in a tumor could result in different treatment approaches.
-
Palliative care/supportive care. Clinical trials are underway to find better ways of reducing symptoms and side effects of current skin cancer treatments to improve comfort and quality of life for patients.
Looking for More About the Latest Research?
If you would like more information about the latest areas of research in non-melanoma skin cancer, explore these related items that take you outside of this guide:
-
To find clinical trials specific to your diagnosis, talk with your doctor or search online clinical trial databases .
-
Visit the Cancer.Net Blog to read about skin cancer research and other related topics.
-
Visit the website of Conquer Cancer, the ASCO Foundation, to find out how to help support cancer research. Please note that this link takes you to a different ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance on how to cope with the physical, emotional, social, and financial changes that cancer and its treatment can bring. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Coping with Treatment
ON THIS PAGE: You will learn more about coping with the physical, emotional, social, and financial effects of cancer and its treatment. Use the menu to see other pages.
Every cancer treatment can cause side effects or changes to your body and how you feel. For many reasons, people do not experience the same side effects even when they are given the same treatment for the same type of cancer. This can make it hard to predict how you will feel during treatment.
As you prepare to start cancer treatment, it is normal to fear treatment-related side effects . It may help to know that your health care team will work to prevent and relieve side effects. This part of cancer treatment is called palliative care or supportive care. It is an important part of your treatment plan, regardless of your age or the stage of disease.
Coping with physical side effects
Common physical side effects from each treatment option for non-melanoma skin cancer are described in the Types of Treatment section. Because skin cancers often occur in areas of the skin that are exposed, the scars that result from treatment can affect a person’s appearance and self-esteem. Learn more about side effects of cancer and its treatment, along with ways to prevent or control them . Changes to your physical health depend on several factors, including the cancer’s extent, the length and dose of treatment, and your general health.
Talk with your health care team regularly about how you are feeling. It is important to let them know about any new side effects or changes in existing side effects. If they know how you are feeling, they can find ways to relieve or manage your side effects to help you feel more comfortable and potentially keep any side effects from worsening.
You may find it helpful to keep track of your side effects so it is easier to talk about any changes with your health care team. Learn more about why tracking side effects is helpful .
Sometimes, side effects can last after treatment ends. Doctors call these long-term side effects. Side effects that occur months or years after treatment are called late effects . Treating long-term side effects and late effects is an important part of survivorship care. Learn more by reading the Follow-up Care section of this guide or talking with your doctor.
Coping with emotional and social effects
You can have emotional and social effects after a cancer diagnosis. This may include dealing with a variety of emotions, such as sadness, anxiety, or anger, or managing your stress level. Sometimes, people find it difficult to express how they feel to their loved ones. Some have found that talking to an oncology social worker, counselor, or member of the clergy can help them develop more effective ways of coping and talking about cancer.
You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your needs.
Coping with the costs of cancer care
Cancer treatment can be expensive. It may be a source of stress and anxiety for people with cancer and their families. In addition to treatment costs, many people find they have extra, unplanned expenses related to their care. For some people, the high cost of medical care stops them from following or completing their cancer treatment plan. This can put their health at risk and may lead to higher costs in the future. Patients and their families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations in a separate part of this website.
Coping with barriers to care
Some groups of people experience different rates of new cancer cases and experience different outcomes from their cancer diagnosis. These differences are called “cancer disparities.” Disparities are caused in part by real-world barriers to quality medical care and social determinants of health , such as where a person lives and whether they have access to food and health care. Cancer disparities more often negatively affect racial and ethnic minorities , people with fewer financial resources , sexual and gender minorities (LGBTQ+) , adolescent and young adult populations , older adults , and people who live in rural areas or other underserved communities .
If you are having difficulty getting the care you need, talk with a member of your health care team or explore other resources that help support medically underserved people .
Talking with your health care team about side effects
Before starting treatment, talk with your doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they likely to happen?
-
What can we do to prevent or relieve them?
-
When and who should we call about side effects?
Be sure to tell your health care team about any side effects that happen during treatment and afterward, too. Tell them even if you do not think the side effects are serious. This discussion should include physical, emotional, social, and financial effects of cancer.
Caring for a loved one with cancer
Family members and friends often play an important role in taking care of a person with non-melanoma skin cancer. This is called being a caregiver. Caregivers can provide physical, practical, and emotional support to the patient, even if they live far away. Being a caregiver can also be stressful and emotionally challenging. One of the most important tasks for caregivers is caring for themselves .
Caregivers may have a range of responsibilities on a daily or as-needed basis, including:
-
Providing support and encouragement
-
Talking with the health care team
-
Giving medications
-
Helping manage symptoms and side effects
-
Coordinating medical appointments
-
Providing a ride to and from appointments
-
Assisting with meals
-
Helping with household chores
-
Handling insurance and billing issues
A caregiving plan can help caregivers stay organized and help identify opportunities to delegate tasks to others. It may be helpful to ask the health care team how much care will be needed at home and with daily tasks during and after treatment. Use this 1-page fact sheet to help make a caregiving action plan. This free fact sheet is available as a PDF, so it is easy to print.
Learn more about caregiving or read the ASCO Answers Guide to Caring for a Loved One With Cancer in English or Spanish .
Looking for More on How to Track Side Effects?
Cancer.Net offers several resources to help you keep track of your symptoms and side effects. Please note that these links will take you to other sections of Cancer.Net:
-
Cancer.Net Mobile: The free Cancer.Net mobile app allows you to securely record the time and severity of symptoms and side effects.
-
ASCO Answers Managing Pain: Get this 32-page booklet about the importance of pain relief that includes a pain tracking sheet to help patients record how pain affects them. The free booklet is available as a PDF, so it is easy to print.
-
ASCO Answers Fact Sheets: Read 1-page fact sheets on anxiety and depression , constipation , diarrhea , rash , and immunotherapy side effects that provide a tracking sheet to record details about the side effect. These free fact sheets are available as a PDF, so they are easy to print, fill out, and give to your health care team.
The next section in this guide is Follow-up Care . It explains the importance of checkups after cancer treatment is finished. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Follow-Up Care
ON THIS PAGE: You will read about your medical care after cancer treatment is completed and why this follow-up care is important. Use the menu to see other pages.
Care for people diagnosed with skin cancer does not end when active treatment has finished. Your health care team will continue to check that the cancer has not come back, manage any side effects, and monitor your overall health. This is called follow-up care.
Your follow-up care may include regular physical examinations, medical tests, or both. Doctors want to keep track of your recovery in the months and years ahead. An important part of your follow-up care will be regular screening for new skin cancers, which should include whole-body skin examinations by a health care professional. This is because many people treated for 1 skin cancer develop other skin cancers later.
Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence, which means that the cancer has come back. Cancer recurs because small areas of cancer cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms. During follow-up care, a doctor familiar with your medical history can give you personalized information about your risk of recurrence. Your doctor will ask specific questions about your health. Some people may have blood tests or imaging tests done as part of regular follow-up care, but testing recommendations depend on several factors, including the type and stage of cancer first diagnosed and the types of treatment given.
The anticipation before having a follow-up test or waiting for test results may add stress to you or a family member. This is sometimes called “scanxiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects
Most people expect to have side effects when receiving treatment. However, it is often surprising to survivors that some side effects may linger beyond the treatment period. These are called long-term side effects. Other side effects called late effects may develop months or even years after treatment has ended. Long-term and late effects can include both physical and emotional changes.
For most people with non-melanoma skin cancer, surgery removes only a small part of the skin. However, if surgery was more extensive, reconstructive services may be needed. People who have had multiple surgeries, particularly on their face, may have a substantially altered appearance. Scars from surgery may be itchy, painful, or limit the ability to move nearby skin. This can be improved by a plastic surgeon or a dermatologist. Rarely, the eyelid may be altered. The eyelid may not close well, and the person may need to use drops to moisten the eye.
When extensive surgery is necessary, the person will need support and possibly the help of a caregiver at home during treatment and recovery. Some of these surgeries are done in several steps and may require a long-term absence from work or other activities. Talk with your health care team, including a social worker, to help plan for this, if necessary.
When radiation therapy is used, there is a small possibility that a second cancer may develop, which may not appear for more than 10 years after treatment. Also, the skin may become thin, discolored, and hard many years after finishing radiation therapy. This can be improved with physical therapy and oral or topical medications prescribed by a dermatologist.
Cancer rehabilitation may be recommended, and this could mean any of a wide range of services, such as physical therapy, occupational therapy, career counseling, pain management, nutritional planning, and/or emotional counseling. The goal of rehabilitation is to help people regain control over many aspects of their lives and remain as independent as possible. Learn more about cancer rehabilitation.
Talk with your doctor about your risk of developing such side effects based on your diagnosis, your individual treatment plan, and your overall health. If you had a treatment known to cause specific late effects, you may have certain physical examinations, scans, or blood tests to help find and manage them.
Keeping personal health records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. ASCO offers forms to help keep track of the cancer treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see a specialist like a dermatologist or oncologist, while others transition back to the care of their primary care doctor or another health care professional. This decision depends on several factors, including the type and stage of cancer, side effects, health insurance rules, and your personal preferences.
If a doctor who was not directly involved in your cancer care will lead your follow-up care, be sure to share your cancer treatment summary and survivorship care plan forms with them and with all future health care providers. Details about your cancer treatment are very valuable to the health care professionals who will care for you throughout your lifetime.
Making healthy lifestyle choices
Many people who are treated for skin cancer lead an active, outdoor lifestyle, and it is very important to take steps to protect your skin from further damage. Participate in outdoor activities before 10:00 AM or after 4:00 PM. When you are outdoors, wear long sleeves, pants, broad-spectrum sunscreen, sunglasses with UV protection, and a wide-brimmed hat to protect against further skin damage. Learn more about protecting your skin from the sun.
People recovering from skin cancer are encouraged to follow established guidelines for good health, such as not smoking, limiting alcohol, eating well, exercising regularly, and managing stress. Regular physical activity can help rebuild your strength and energy level. Your health care team can help you create an appropriate exercise plan based on your needs, physical abilities, and fitness level. Learn more about making healthy lifestyle choices .
The next section offers Questions to Ask the Health Care Team to help start conversations with your cancer care team. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Questions to Ask the Health Care Team
ON THIS PAGE: You will find some questions to ask your doctor or other members of the health care team to help you better understand your diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with the health care team is important to make informed decisions about your health care. These suggested questions are a starting point to help you learn more about your cancer care and treatment. You are also encouraged to ask additional questions that are important to you. You may want to print this list and bring it to your next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your care. It may also be helpful to ask a family member or friend to come with you to appointments to help take notes.
Questions to ask before a biopsy
-
What should I expect during and after a skin biopsy?
-
Will the biopsy remove all of the lesion?
-
Will there be a scar? If so, what will it look like?
-
Are there any other risks to performing this biopsy?
-
Are there other lesions that should be biopsied?
-
Which laboratory will examine this biopsy sample? Is there a pathologist who specializes in skin cancer working there?
Questions to ask after getting a diagnosis
-
What type of skin cancer do I have?
-
Can you explain my pathology report (laboratory test results) to me?
-
Are more tests needed to find out if the cancer has spread?
Questions to ask about choosing a treatment and managing side effects
-
What are my treatment options?
-
What clinical trials are available for me? Where are they located, and how do I find out more about them?
-
What treatment plan do you recommend? Why?
-
What is the goal of each treatment? Is it to eliminate the cancer, help me feel better, or both?
-
Are there other ways to treat the cancer, in addition to the recommended treatment?
-
What are the possible side effects of each treatment, both in the short term and the long term?
-
Could this treatment cause changes to my appearance?
-
Who will be part of my health care team, and what does each member do?
-
Who will be leading my overall treatment?
-
How will this treatment affect my daily life? Will I be able to work, exercise, and perform my usual activities?
-
If I’m worried about managing the costs of cancer care, who can help me?
-
What support services are available to me and my family?
-
If I have questions or problems, who should I call?
Questions to ask about having surgery
-
What type of surgery will I have?
-
How long will it take to remove the lesion?
-
How will the surgical area resulting from the removal of the lesion be closed, repaired, or reconstructed?
-
Can you describe what my recovery from surgery will be like? Are there limitations to activities? If so, for how long?
-
Will there be ongoing pain after the cancer is removed? If so, what types of pain management programs, such as medications or relaxation techniques, are available?
-
What will the scar look like after surgery? How long will it take to heal?
-
Who should I contact about any side effects I experience? And how soon?
-
Are there any other possible long-term effects of having this surgery?
Questions to ask about having radiation therapy
-
What type of radiation therapy is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about having therapies using medications
-
What type of medication is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
Will I receive this treatment at a hospital or clinic? Or will I take it at home?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about planning follow-up care
-
What is the chance that the cancer will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the cancer treatment I received?
-
How often should I have checkups to watch for other skin cancers?
-
What other follow-up tests will I need, and how often will those tests be needed?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
Who will be leading my follow-up care?
-
What steps should I take to prevent future skin cancers?
-
What support services are available to me? To my family?
The next section in this guide is Additional Resources . It offers more resources on this website that may be helpful to you. Use the menu to choose a different section to read in this guide.
Skin Cancer (Non-Melanoma) - Additional Resources
ON THIS PAGE: You will find some helpful links to other areas of Cancer.Net that provide information about cancer care and treatment. This is the final page of Cancer.Net’s Guide to Non-Melanoma Skin Cancer. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of cancer, both for the person diagnosed and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Here are a few links to help you explore other parts of Cancer.Net:
-
Search for a cancer specialist in your local area using this free database of doctors from the American Society of Clinical Oncology.
-
Learn what medical phrases and terms used in cancer care and treatment mean.
-
Read more about the first steps to take when you are diagnosed with cancer .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of cancer care.
-
Learn more about coping with the emotions that cancer can bring, including those within a family or a relationship.
-
Find a national, not-for-profit advocacy organization that may offer additional information, services, and support for people with skin cancer.
-
Explore what to do when you finish active treatment .
-
Download Cancer.Net Mobile , a free app that includes a symptom and side effect tracker, medication reminders, and other interactive resources.
-
To find a range of information and insights from different voices on timely cancer topics, visit the Cancer.Net Blog .
-
Watch Cancer.Net videos with ASCO experts explaining the basics of cancer treatment, side effects, survivorship, clinical trials, caregiving, and more.
This is the end of Cancer.Net’s Guide to Non-Melanoma Skin Cancer. Use the menu to choose a different section to read in this guide.













