Pancreatic Cancer - Introduction
ON THIS PAGE: You will find some basic information about this disease and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Pancreatic Cancer. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
Pancreatic cancer is a disease in which healthy cells in the pancreas stop working correctly and grow out of control. These cancerous cells can build up and form a mass called a tumor. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. As it grows, a pancreatic tumor can affect the function of the pancreas, grow into nearby blood vessels and organs, and eventually spread to other parts of the body through a process called metastasis.
About the pancreas
The pancreas is a pear-shaped glandular organ about the size of a hand. It is located in the upper center of the abdomen between the stomach and the spine. It is made up of 2 major components:
-
The exocrine component is made up of ducts and small sacs called acini on the end of the ducts. This part of the pancreas makes specialized proteins called enzymes that are released into the small intestine to help the body digest and break down food, particularly fats.
-
The endocrine component is made up of cells lumped together in different locations within this part of the pancreas, called islets of Langerhans. These cells make specific hormones, the most important of which is insulin. Insulin is the substance that helps control the amount of sugar in the blood. This portion of the pancreas also makes other hormones, such as glucagon, somatostatin, pancreatic polypeptide (PP), and vasoactive intestinal peptide (VIP). Each of these hormones plays an important role in regulating the body’s metabolism.
The pancreas is made up of the head, body, and tail. Pancreatic cancers most commonly arise from the head of the pancreas.
Types of pancreatic cancer
There are several types of pancreatic cancer, mainly depending on whether the cancer began in the exocrine or endocrine component. Pancreatic cancers are considered to be solid tumors.
Exocrine tumors. These are the most common type of pancreatic cancer. Most people refer to this type of cancer simply as pancreatic cancer. The most common type of exocrine tumor is called adenocarcinoma. Adenocarcinoma is not unique to the pancreas, as it develops in the glandular tissue that lines certain internal organs. When these tumors occur in the pancreas, they usually start in the ducts of the pancreas, called ductal adenocarcinoma. Much less commonly, if the tumor begins in the acini, it is called acinar cell carcinoma.
An increasingly common diagnosis is called intraductal papillary mucinous neoplasm (IPMN). An IPMN is a tumor that grows within the ducts of the pancreas and makes a thick fluid called mucin. Pancreatic ducts carry fluids from the pancreas to the bowels to help with digestion. IPMN is not cancerous when it begins, but it could become cancerous over time if not treated. Sometimes, an IPMN has already worsened and has become a cancer by the time it is diagnosed.
Much rarer types of exocrine pancreatic tumors include acinar cell carcinoma, adenosquamous carcinoma, colloid carcinoma, giant cell tumor, hepatoid carcinoma, mucinous cystic neoplasms, pancreatoblastoma, serous cystadenoma, signet ring cell carcinoma, solid and pseudopapillary tumors, squamous cell carcinoma, and undifferentiated carcinoma.
Endocrine tumors. These are also called pancreatic neuroendocrine tumors (PNETs) or islet cell tumors. They are much less common than exocrine tumors, making up about 7% of all pancreatic cancers. This type of tumor is very different than what most people refer to as pancreatic cancer. A pancreatic neuroendocrine tumor can be functioning or nonfunctioning. A functioning tumor makes hormones. A nonfunctioning tumor does not make hormones. A functioning neuroendocrine tumor is named based on the hormone the cells normally make. These include:
-
Insulinoma
-
Glucagonoma
-
Gastrinoma
-
Somatostatinoma
-
VIPomas
-
PPomas
To learn more about tumors that start in the endocrine component of the pancreas, read Cancer.Net's separate guide about
neuroendocrine tumors of the pancreas
.
Sometimes, other types of cancer can begin in the pancreas, such as
lymphoma
and
sarcoma
.
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
ASCO Answers Fact Sheet: Read a 1-page fact sheet that offers an introduction to pancreatic cancer. This free fact sheet is available as a PDF, so it is easy to print.
-
Cancer.Net En Español: Read about pancreatic cancer in Spanish . Infórmase sobre cáncer pancreático en español .
-
Find a Cancer Doctor. Search for a cancer specialist in your local area using this free database of doctors from the American Society of Clinical Oncology (ASCO).
-
Cancer Terms. Learn what medical phrases and terms used in cancer care and treatment mean.
The next section in this guide is Statistics . It helps explain the number of people who are diagnosed with pancreatic cancer and general survival rates. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Statistics
ON THIS PAGE: You will find information about the estimated number of people who will be diagnosed with pancreatic cancer each year. You will also read general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with cancer are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this cancer and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for you individually. The original sources for these statistics are provided at the bottom of this page.
How many people are diagnosed with pancreatic cancer?
In 2023, an estimated 64,050 adults (33,130 men and 30,920 women) in the United States will be diagnosed with pancreatic cancer. The disease accounts for approximately 3% of all cancers. Pancreatic cancer is the eighth most common cancer in women and the tenth most common cancer in men. In both men and women, the number of new cases of pancreatic cancer have gone up by around 1% each year since the late 1990s. Worldwide, an estimated 495,773 people were diagnosed with pancreatic cancer in 2020.
It is estimated that 50,550 deaths (26,620 men and 23,930 women) from this disease will occur in the United States in 2023. It is the fourth leading cause of cancer death in both men and women. Pancreatic cancer accounts for 7% of all cancer deaths. Since the late 1990s, the death rate has very slowly increased by 0.2% per year in men and stayed steady in women. In 2020, an estimated 466,003 people worldwide died from pancreatic cancer.
As explained in the
Introduction
, more than 90% of pancreatic cancers are exocrine adenocarcinoma.
What is the survival rate for pancreatic cancer?
There are different types of statistics that can help doctors evaluate a person’s chance of recovery from pancreatic cancer. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having cancer may affect life expectancy. Relative survival rate looks at how likely people with pancreatic cancer are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this cancer.
Example: Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) will be alive in 5 years.
It is important to remember that statistics on the survival rates for people with pancreatic cancer are only an estimate. They cannot tell an individual person if cancer will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
The 5-year relative survival rate for pancreatic cancer in the United States is 12%.
The survival rates for pancreatic cancer vary based on several factors. These include the stage of cancer, a person’s age and general health, and how well the treatment plan works. Pancreatic neuroendocrine tumors (PNETs) often have a better prognosis, which is the chance of recovery, both in terms of the chance of a cure and in terms of life expectancy if not cured.
Pancreatic cancer is often difficult to diagnose . This is because there are no validated, specific screening tests that can easily and reliably find early-stage pancreatic cancer in people who do not show symptoms. Furthermore, people with pancreatic cancer often do not have clearly identified symptoms in the early stages of the disease. This means it is often not found until later stages when the cancer can no longer be removed with surgery and/or has spread from the pancreas to other parts of the body.
If the cancer is detected at an early stage when surgical removal of the tumor is possible, the 5-year relative survival rate is 44%. About 12% of people are diagnosed at this stage. If the cancer has spread to surrounding tissues or organs, the 5-year relative survival rate is 15%. For the 52% of people who are diagnosed after the cancer has spread to a distant part of the body, the 5-year relative survival rate is 3%.
Experts measure relative survival rate statistics for pancreatic cancer every 5 years. This means the estimate may not reflect the results of advancements in how pancreatic cancer is diagnosed or treated from the last 5 years. Talk with your doctor if you have any questions about this information. Learn more about understanding statistics .
Statistics adapted from the American Cancer Society's (ACS) publication, Cancer Facts & Figures 2023, the ACS website, the International Agency for Research on Cancer website, and the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. (All sources accessed March 2023.)
The next section in this guide is Medical Illustrations . It offers drawings of body parts often affected by pancreatic cancer. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Medical Illustrations
ON THIS PAGE : You will find a drawing of the main body parts affected by pancreatic cancer. Use the menu to see other pages.
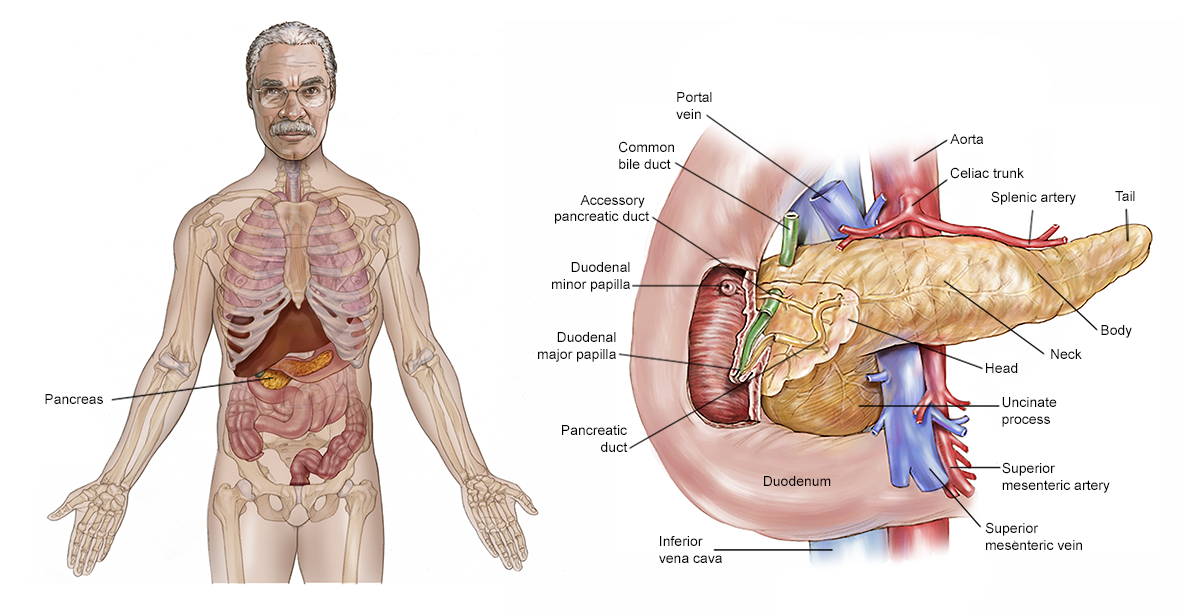
Copyright 2022 American Society of Clinical Oncology. Robert Morreale.
The next section in this guide is Risk Factors . It describes the factors that may increase the chance of developing pancreatic cancer. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Risk Factors
ON THIS PAGE: You will find out more about the factors that increase the chance of developing pancreatic cancer. Use the menu to see other pages.
What are the risk factors for pancreatic cancer?
A risk factor is anything that increases a person’s chance of developing cancer. These risk factors can be out of your control, such as genetics or age, while others can be in your control, such as smoking. Although risk factors often influence the development of cancer, most do not directly cause cancer. Some people with 1 or more risk factors may never develop cancer, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor and health care team may help you make more informed lifestyle and health care choices.
Often, the cause of pancreatic cancer is not known. A person with an "average risk" of pancreatic cancer has about a 1% chance of developing the disease. Generally, most pancreatic cancers (about 90%) are considered sporadic. Also called somatic mutations, this means the genetic changes that led to cancer developed by chance after a person was born. There is no risk of passing these genetic changes on to one’s children.
Inherited pancreatic cancers are less common (about 10% of all pancreatic cancers). They occur when gene mutations or changes are passed within a family from 1 generation to the next (see below), raising the risk of pancreatic cancer. These are also called germline mutations. See below for specific inherited conditions that increase a person's risk of pancreatic cancer. To learn more about inherited pancreatic cancers and their relationship to other types of cancers with which they share genetic mutations, you can contact a Pancreatic Cancer Familial Registry.
Early detection and prevention for any cancer can lead to the most favorable long-term patient outcomes. Researchers in pancreatic cancer continue to search for answers to develop a routine screening method for the general population, as none currently exists.
In general, the following factors may raise a person’s risk of developing pancreatic cancer:
-
Age. The risk of developing pancreatic cancer increases with age. Most people who develop pancreatic cancer are older than 45. In fact, 90% are older than 55 and 70% are older than 65. However, adults of any age can be diagnosed with pancreatic cancer, as can children rarely.
-
Sex. More men are diagnosed with pancreatic cancer than women (see Statistics ).
-
Race/ethnicity. Black people are more likely than Asian, Hispanic, or White people to develop pancreatic cancer. People of Ashkenazi Jewish heritage are also more likely to develop pancreatic cancer (see "Family history," below).
-
Smoking. People who smoke tobacco are 2 to 3 times more likely to develop pancreatic cancer than those who don’t. Learn more about quitting smoking .
-
Obesity, diet, and alcohol. Regularly eating foods high in fat is a risk factor for pancreatic cancer. Research has shown that obese and even overweight people have a higher risk of being diagnosed with and dying from pancreatic cancer. Chronic, heavy alcohol use can also increase the risk of pancreatic cancer, most likely by causing recurrent pancreatitis, which is repeated inflammation of the pancreas. Learn more about how cancer risk relates to obesity , food choices , and drinking alcohol .
-
Diabetes. Many studies have indicated that diabetes increases the risk of developing pancreatic cancer, especially when a person has had diabetes for many years. In addition, suddenly developing diabetes later in adulthood, sometimes called new-onset or adult-onset diabetes, can be an early symptom of pancreatic cancer. However, it is important to remember that not all people who have diabetes or who are diagnosed with diabetes as adults develop pancreatic cancer. Talk with your health care team and genetic counselor if you have diabetes .
-
Family history. Pancreatic cancer may run in the family and/or may be linked with genetic conditions that increase the risk of other types of cancer. This is called familial pancreatic cancer . Keeping track of your family's history of health conditions is a recommended practice. This should include siblings of your parents and grandparents through current generations of your family. You and your family may be at an increased risk if 2 or more first-degree relatives or at least 3 members of the family have been diagnosed with pancreatic cancer. First-degree relatives include parents, children, and siblings. The American Society of Clinical Oncology (ASCO) encourages people diagnosed with pancreatic adenocarcinoma to talk with their doctor about their family history of cancer. Even without a strong family history of cancer, people diagnosed with pancreatic adenocarcinoma are recommended to undergo genetic testing for hereditary pancreatic cancer. People with a family history of other cancer types that have genetic mutations in common with pancreatic cancer may also want to consider having discussions with a genetic counselor. Talk with your health care team about whether genetic testing is right for you and whether you should speak with a genetic counselor .
Families and individuals with inherited genetic changes, called mutations or alterations, in certain genes, including BRCA1, BRCA2, PALB2, CDKN2A, ATM, MLH1, MSH2, MSH6, PMS2, STK11/LKB1, P16, P53, PRSS1, FANC-C, FANC-G, or EPCAM, are at increased risk for pancreatic cancer. Some of these genes are responsible for causing the hereditary syndromes described below.
There are specialized research studies looking at pancreatic screening tools, such as magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS), for these high-risk individuals. These tools are described in further detail in the Diagnosis section. Talk with your health care team about the screening options.
-
Hereditary syndromes. Certain hereditary syndromes are present in families that significantly increase family members' risk of pancreatic cancer, as well as other types of cancer. These include the following:
-
Hereditary pancreatitis (HP) , which is a condition associated with recurrent pancreatitis and an increased risk of pancreatic cancer
-
Peutz-Jeghers syndrome (PJS)
-
Familial malignant melanoma and pancreatic cancer (FAMM-PC)
-
Hereditary breast and ovarian cancer (HBOC) syndrome
-
Lynch syndrome
People with the following inherited conditions may also have a higher risk of pancreatic cancer:
-
Li-Fraumeni syndrome (LFS)
-
Familial adenomatous polyposis (FAP)
-
-
Chronic pancreatitis. Pancreatitis is the inflammation of the pancreas. It is typically a painful pancreatic disease. Some research suggests that having chronic pancreatitis may increase the risk of developing pancreatic cancer.
-
Chemicals. Exposure to certain chemicals, such as pesticides, benzene, certain dyes, and petrochemicals, may increase the risk of developing pancreatic cancer.
-
Bacteria. A common bacterium called Helicobacter pylori , also called H. pylori , causes inflammation and ulcers in the stomach. Infection with H. pylori increases the risk of both stomach cancer and pancreatic cancer. However, the risk of developing pancreatic cancer is not as high as the risk of developing stomach cancer.
-
Hepatitis B infection. Hepatitis viruses infect the liver. One study has shown that a previous hepatitis B infection was twice as common in people with pancreatic cancer than in people without the cancer. More research is needed to learn more about this link.
-
Cirrhosis. Cirrhosis develops when liver cells are damaged and are replaced by scar tissue. Most cirrhosis in the United States is caused by drinking a lot of alcohol regularly. Other causes are viral hepatitis (see above), too much iron in the liver from a disease called hemochromatosis, and some other rare types of chronic liver disease. Cirrhosis most commonly results in liver cancer , but it can also cause pancreatic cancer.
The next section in this guide is Symptoms and Signs . It explains what changes or medical problems pancreatic cancer can cause. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Symptoms and Signs
ON THIS PAGE: You will find out more about the changes and medical problems that can be a sign of pancreatic cancer. Use the menu to see other pages.
What are the symptoms and signs of pancreatic cancer?
People with pancreatic cancer may experience one or more of the following symptoms or signs. Symptoms are changes that you can feel in your body. Signs are changes in something measured, like taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. Sometimes, people with pancreatic cancer do not have any of the symptoms and signs described below. Or, the cause of a symptom or sign may be a medical condition that is not cancer.
Doctors often say that pancreatic cancer is a “silent disease” because there are not many noticeable symptoms early on. Also, there are currently no specific tests that can reliably find the cancer for people who do not have symptoms. When people do have symptoms, they are often similar to the symptoms of other medical conditions, such as an ulcer or pancreatitis (see Risk Factors ). As the cancer grows, symptoms may include:
-
Yellow skin (including yellowing of the gums and inner lips) and/or eyes, darkening of the urine, itching, and clay-colored stool, which are signs of jaundice caused by a blockage of the bile ducts
-
Pain in the upper abdomen, back, or arms
-
Painful swelling of an arm or leg due to a blood clot
-
Burning feeling in the stomach or other gastrointestinal discomforts
-
Stomach bloating
-
Floating and/or oily stools with a particularly bad odor and an unusual color due to the body not digesting fats well, called malabsorption
-
Weakness
-
Loss of appetite
-
Nausea and vomiting
-
Chills and sweats
-
Fever
-
Unexplained weight loss
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will try to understand what is causing your symptom(s). They may do an exam and order tests to understand the cause of the problem, which is called a diagnosis.
If cancer is diagnosed, relieving symptoms remains an important part of cancer care and treatment. Managing symptoms may also be called "palliative and supportive care," which is not the same as hospice care given at the end of life. This type of care focuses on managing symptoms and supporting people who face serious illnesses, such as cancer. You can receive palliative and supportive care at any time during cancer treatment. Learn more in this guide’s section on Coping with Treatment .
Be sure to talk with your health care team about the symptoms you experience, including any new symptoms or a change in symptoms. You may also want to consider keeping a written log or notebook about your symptoms with specific details and dates to assist your discussions with your health care team.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Diagnosis
ON THIS PAGE: You will find a list of common tests, procedures, and scans that doctors use to find the cause of a medical problem. Use the menu to see other pages.
Doctors use many tests to find, or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If the cancer has spread, it is called metastasis. Doctors may also do tests to learn which treatments could work best.
For most types of cancer, a biopsy is the only sure way for the doctor to know if an area of the body has cancer. However, a cancer diagnosis is also possible without a fully confirmed biopsy. In a biopsy, the doctor takes a small sample of tissue from the suspected area of the cancer for testing in a laboratory. Biopsies for pancreatic cancer are known to often be difficult to obtain tissue samples for because of the location of the pancreas. And, pancreatic tumors are often initially smaller and more spread out than other types of tumors, which may be described as "diffuse." Sometimes the doctor can get a tissue sample, but the sample might contain a very small amount of tumor cells and might not be enough to make a definitive diagnosis. If a biopsy is inconclusive or not possible, the doctor may suggest other tests that will help make a diagnosis.
How pancreatic cancer is diagnosed
There are different tests used for diagnosing pancreatic cancer. Not all tests described here will be used for every person. Your doctor may consider these factors when choosing a diagnostic test:
-
The type of cancer suspected
-
Your signs and symptoms
-
Your age, general health, and family history
-
The results of earlier medical tests
If a doctor suspects that a person has pancreatic cancer, they will first ask about the person's medical history and family history. Then, they will examine the person to look for signs of the disease . An appropriate and timely diagnosis is very important. If possible, tests should be done at a medical center that has experience with the disease. The tests described below may be used when pancreatic cancer is suspected. However, the diagnosis should be confirmed with a sample of tissue from the tumor taken during a biopsy or surgery. These tests are described more below.
General tests
-
Physical examination. The doctor will examine your skin, tongue, and eyes to see if they are yellow, which is a sign of jaundice. Jaundice can be caused by a tumor in the head of the pancreas blocking the normal flow of a substance called bile, which is produced in the liver. However, many people with pancreatic cancer do not have jaundice when the cancer is diagnosed. Your doctor will also feel your abdomen for changes caused by the cancer, although the pancreas itself, which is located in the back of the upper abdomen, can rarely be felt. An abnormal buildup of fluid in the abdomen, called ascites , may be another sign of cancer. The doctor will also examine your abdomen to determine if you have pain in the upper portion of your abdomen just below your breastbone.
-
Blood tests. The doctor may take samples of blood to check for abnormal levels of bilirubin and other substances. Bilirubin is a chemical that may reach high levels in people with pancreatic cancer due to blockage of the common bile duct by a tumor. There are many other non-cancerous causes of an elevated bilirubin level, such as hepatitis, gallstones, or a common infection called mononucleosis, or "mono."
Carbohydrate antigen 19-9 (CA19-9) is a tumor marker. A tumor marker is a substance produced by a tumor that may be found at higher levels if cancer is present. Tumor markers are typically found in the blood, urine, stool, and other bodily fluids. CA19-9 levels are often increased in people with pancreatic cancer, although some patients have normal CA19-9 levels. CA19-9 levels often become higher as the cancer grows or spreads. CA 19-9 should not be used as the only test to diagnose pancreatic cancer because high levels of CA 19-9 can also be a sign of other conditions. For example, other types of cancer, such as colorectal, liver, and esophageal cancers, can increase CA 19-9. And noncancerous conditions, such as diabetes, pancreatitis, cirrhosis of the liver, and a non-cancerous blockage of the common bile duct, may also increase CA 19-9.
Imaging tests
Imaging tests show pictures of the inside of the body. They can help doctors find out where the cancer is located and whether it has spread from the pancreas to other parts of the body. Imaging tests may also be used to monitor whether the cancer is growing. Pancreatic cancer often does not develop as a single large tumor, which means it can sometimes be difficult to see on imaging tests. However, newer computed tomography scanners (see below) produce better, clearer images that can make it easier to find a tumor. A radiologist is a doctor who specializes in interpreting imaging tests.
-
Computed tomography (CT or CAT) scan. A CT scan takes pictures of the inside of the body using high-speed x-rays taken from different angles. A computer combines these pictures into a detailed, multi-dimensional image (typically 3-dimensional or more) that shows any abnormalities or tumors. A CT scan can be used to determine the size and location of the primary tumor and evaluate the possibility of spread to lymph nodes or other parts of the body. Typically, a special dye called a contrast medium is given before the scan to provide better detail on the image. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow.
Many cancer centers use a special CT scan method called a pancreatic protocol CT scan. This method focuses on taking pictures of the pancreas at specific times after the intravenous (IV) injection of contrast medium to find out exactly where the tumor is in relation to nearby organs and blood vessels. The results of this test can help decide if the tumor could be removed with surgery.
The American Society of Clinical Oncology (ASCO) recommends that people with metastatic pancreatic cancer should get a CT scan done of their chest, abdomen, and pelvis to evaluate the extent of the cancer. A CT scan or other imaging may also be used 2 to 3 months after standard treatment begins to evaluate treatment effectiveness.
-
Positron emission tomography (PET) scan or PET-CT scan. A PET scan creates multi-colored pictures of organs and tissues inside the body. A PET scan is usually combined with a CT scan (see above), called a PET-CT scan . Sometimes, it may be combined with magnetic resonance imaging (MRI; see below). However, you may hear your doctor refer to this procedure just as a PET scan. A small amount of a radioactive sugar substance called a tracer is injected into the patient’s body. The most common tracer used in pancreatic cancer PET scans is fluorodeoxyglucose (FDG). This sugar substance is taken up by cells that use the most energy and will cause them to "light up" much brighter on the PET scan. Because cancer tends to use energy actively, it absorbs more of the radioactive tracer substance. However, the amount of radiation in the substance is intentionally designed to be too low to be harmful. There are also non-cancerous reasons an area can light up, such as an infection or active organ functioning. A PET scanner detects the injected substance to produce images of the inside of the body. The combination provides a more complete picture of the area being evaluated. A PET scan alone should never be used instead of a high-quality, high-speed CT scan. PET scans differ from CT scans in that CT scans are looking at the tumor in relation to your anatomy, while PET scans are attempting to measure metabolic activity. The 2 tests are typically used together for pancreatic cancer.
-
Endoscopic retrograde cholangiopancreatography (ERCP). This procedure is performed by a gastroenterologist. A gastroenterologist is a doctor who specializes in the gastrointestinal tract, including the stomach, intestines, and similar organs. The doctor will put a thin, lighted tube called an endoscope through the mouth and stomach into the small intestine. Then, a smaller tube called a catheter is passed through the endoscope and into the bile ducts and pancreatic ducts. Dye is injected into the ducts, and the doctor takes x-rays that can show whether a duct is compressed or narrowed. Often, a plastic or metal stent can be placed across the obstructed bile duct during ERCP to help relieve any jaundice. Samples of the tissue can be taken during this procedure and can sometimes help confirm the diagnosis of cancer. The patient is lightly sedated during this procedure. ERCP is generally used to place bile duct stents and not commonly used for diagnosis.
-
Ultrasound. An ultrasound creates a picture of the internal organs using sound waves. There are 2 types of ultrasound devices:
-
A transabdominal ultrasound device is placed against the outside of the abdomen and is slowly moved around by the doctor to produce an image of the pancreas and surrounding structures.
-
An endoscopic ultrasound (EUS) device is a thin, lighted tube that is passed through the patient's mouth and stomach and down into the small intestine. It is slowly moved around the area to take a picture of the pancreas. This procedure is very specialized and requires a gastroenterologist who has special training in this area. EUS is generally done under sedation, so the patient sleeps through the procedure. A biopsy (see below) may also be done at the same time as this procedure.
-
-
Percutaneous transhepatic cholangiography (PTC). In this x-ray procedure, a thin needle is inserted through the skin and into the liver. A dye is injected through the needle, so the bile ducts show up on x-rays. By looking at the x-rays, the doctor can tell whether there is a blockage of the bile ducts.
-
Magnetic resonance imaging (MRI). An MRI produces detailed images of the inside of the body using magnetic fields, not x-rays. MRI can be used to measure the tumor’s size. A special dye called a contrast medium is given before the scan to create a clearer picture. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow. Magnetic resonance cholangiopancreatography (MRCP) is a specialized type of MRI using computer software developed specifically to examine pancreatic issues, such as ductal blockages and cysts.
Biopsy and tissue tests
-
Biopsy. A biopsy is the only way to make a definite diagnosis, even if other tests can suggest that cancer is present. During biopsy, a small amount of tissue is removed for examination under a microscope. A pathologist analyzes the sample(s). A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. For pancreatic cancer, the pathologist may often have specific experience in looking at pancreatic cancer biopsy samples. There are a couple of different ways to collect a tissue sample:
-
Fine needle aspiration (FNA). An FNA uses a thin needle that is inserted into the pancreas to suction out cells. This is typically done by EUS (see above) or through the skin, called percutaneously, guided by a CT scan.
-
Core needle biopsy. This is used to collect a larger piece of tissue, which may be helpful for biomarker or genetic testing of the tumor (see below). However, a core needle biopsy has higher risks than an FNA, including pancreatitis and bleeding. It should be performed by a gastroenterologist who has been specifically trained and has significant experience in performing EUS.
If the cancer has spread to other organs, a biopsy may also be needed from 1 of these other areas, such as the liver. Again, this can be through the skin, as explained above, or by surgery, which is less common. This type of surgery can be done through a larger incision in the abdomen, called a laparotomy. Or, it can be done using much smaller incisions that provide openings for a tiny camera and surgical instruments, called a laparoscopic approach.
Occasionally, a biopsy may show that there are no cancer cells in the area tested even if there are. This result is called a “false negative" and may also be described as being "inconclusive." This can happen because the area contains inflammation, fibrosis (scar-like tissue), and/or a diffuse tumor, all of which can make the cancer cells harder to find. In general, before a patient starts treatment, every effort is made to confirm that cancer is present, even if this means that multiple biopsies are needed. An exception is for patients with a mass located in a single area of the pancreas that can be removed with surgery even if a biopsy is not performed or the biopsy does not show cancer cells. Another exception may be when several signs and symptoms are present, such as weight loss, pain, ascites, and jaundice, that present a compelling case for a cancer diagnosis.
-
-
Biomarker, or molecular, testing of the tumor. Your doctor may recommend, and you may request, additional molecular tests to be performed on the tumor sample to identify specific mutations, genetic alterations, expression of certain proteins, and other molecular features unique to the tumor. Some of these tests can be done in your local hospital laboratory. For other tests, the sample may need to be sent to an independent laboratory for analysis.
Examples of molecular testing that should be performed include looking for evidence of high microsatellite instability (MSI-high) or defective mismatch repair (dMMR); for mutations in the BRCA gene, as well as other genes involved in DNA damage repair; and for a specific genetic alteration called an NTRK fusion. These tests may help doctors determine your treatment options , including immunotherapy and targeted therapy. However, these findings are not common in pancreatic tumors. The most common genes that are mutated in pancreatic cancer include KRAS, p16/CDKN2A, TP53, and SMAD4/DPC4. There are currently no approved drugs that target these specific mutations, aside from 1 drug that targets a rare type of KRAS mutation. However, more research is being done in this area.
Molecular testing can be commonly referred to as “testing for targeted therapies," "personalized medicine," "precision medicine," or "next generation sequencing." This field of science and treatment is rapidly growing and is an area of increasing interest, scientific focus, and research progress. It is helpful to find out the type and amount of tumor sample needed for these tests and if they are covered by your health insurance. You may need to have another biopsy to get a large enough tissue sample for more extensive testing. Depending on the type of testing, a blood test sometimes referred to as a " liquid biopsy " can provide information on some of the molecular or genetic features of your cancer by analyzing the DNA shed by tumor cells into the bloodstream, known as circulating tumor DNA (ctDNA). Know that these results sometimes take weeks to return, and you do not necessarily wait for the results before starting treatment.For tests such as drug assays, talk with your doctor about the potential information they could provide that would help plan your treatment and whether such tests are covered by your insurance. It is important to discuss these options in advance with the health care professional who will be performing the procedure for the diagnosis. This is to ensure the health care team and technicians have the proper instructions for the procedure should tumor testing be involved.
People who have surgery may also choose to donate parts of the tumor that are not needed for their diagnosis or cancer care so the samples can be used to further pancreatic cancer research. (Learn more about biospecimens in cancer research in a separate article on this website.)
-
Germline testing. It is now recommended that all people with a diagnosis of pancreatic cancer be considered for germline testing (see Risk Factors ). This means testing a blood or saliva sample to look for mutations in a person's DNA that may indicate a hereditary predisposition to cancer. This is typically performed in addition to a visit with a genetic counselor. If a person is found to be a carrier for particular genetic mutations, this may help guide the treatment decisions if pancreatic cancer is diagnosed. It would also signal that their family members may want to consider genetic testing and participation in a pancreatic cancer family registry.
After diagnostic tests have been performed, your doctor will review the results with you, including the exact type of cancer you have, how much the cancer has grown and spread (called the stage), and the options for treatment. You may request copies of all test results and images for your own personal medical records .
Diagnostic and follow-up tests can cause anxiety while waiting for results. This may be called " scanxiety ." Sometimes, with today’s technology, patients may get access to test results before their doctor has seen the results and has had a chance to discuss the results with them. It is important to allow your doctor to review and assess your results before they discuss them with you so they can help guide you with appropriate care.
The next section in this guide is Stages . It explains the system doctors use to describe the extent of the disease. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Stages
ON THIS PAGE: You will learn about how doctors describe a cancer’s growth or spread. This is called the stage. Use the menu to see other pages.
READ MORE BELOW:
-
What is cancer staging?
-
Resectable (localized)
-
Borderline resectable
-
Locally advanced
-
Metastatic
-
TNM staging system
-
Stage groups for pancreatic cancer
What is cancer staging?
Staging is a way of describing where the cancer is located, if or where it has spread, and whether it is affecting other parts of the body.
Staging is typically described in pathology and diagnostic reports. Doctors use diagnostic tests to find out the cancer's stage, so staging may not be complete until all of the tests are finished. Knowing the stage helps the doctor recommend the best kind of treatment; can help predict a patient's prognosis, which is the chance of recovery; and can help identify clinical trials that may be treatment options. There are different stage descriptions for different types of cancer. It is important for the staging to be done at a medical center with experience in diagnosing and staging pancreatic cancer.
Doctors use several systems to stage pancreatic cancer. The method used to stage most other cancers, called the "TNM staging system," is not often used for pancreatic cancer. However, for completeness, TNM is discussed further below. TNM stands for tumor/nodes/metastasis.
The more common way to classify pancreatic cancer is to classify a tumor into 1 of 4 categories, based on whether it can be removed with surgery and where it has spread. These categories are described in detail below, followed by descriptions of the TNM staging system and stage groups for pancreatic cancer.
Return to top
Resectable (localized)
This type of pancreatic cancer can be surgically removed. Surgery is often done right after diagnosis. Sometimes, additional treatment may be recommended before surgery. The tumor may be located only in the pancreas or extend beyond it, but it has not grown into important arteries or veins in the area. There is no evidence that the tumor has spread to areas outside of the pancreas. Approximately 10% to 15% of patients are diagnosed with this stage.
Return to top
Borderline resectable
This category describes a tumor that may be difficult or not possible to remove surgically when it is first diagnosed, but if chemotherapy and/or radiation therapy is able to shrink the tumor first, surgery may be possible to remove the tumor later with negative margins. A "negative margin" means that no visible cancer cells are left behind in the body.
Return to top
Locally advanced
This type of pancreatic cancer is still located only in the area around the pancreas, but it cannot be surgically removed because it has grown into or close to nearby arteries, veins, or organs. This means that it cannot be removed with surgery because the risk of damaging these nearby structures is too high. There are no signs that it has spread to any distant parts of the body. Approximately 35% to 40% of patients are diagnosed with this stage.
Return to top
Metastatic
The tumor has spread beyond the area of the pancreas and to other organs, such as the liver, lungs, or distant parts of the abdomen. Approximately 45% to 55% of patients are diagnosed with this stage.
By classifying each cancer into 1 of these categories, the health care team can plan the best treatment strategy.
Return to top
TNM staging system
Doctors frequently use a tool called the TNM system to stage other types of cancer. Using this system, doctors generally classify a tumor during surgery. However, many patients with pancreatic cancer do not receive surgery. Therefore, the TNM system is not used as much for pancreatic cancer as it is for other cancers.
For the TNM system, doctors use the results from diagnostic tests, scans, and surgery to answer these questions:
-
Tumor (T): How large is the primary tumor? Where is it located?
-
Node (N): Has the tumor spread to the lymph nodes? If so, where and to how many?
-
Metastasis (M): Has the cancer spread to other parts of the body? If so, where and by how much?
The results are combined to determine the stage of cancer for each person. There are 5 stages: stage 0 (zero) and stages I through IV (1 through 4). The stage provides a common way of describing the cancer, so doctors can work together to plan the best treatments. Here are more details on each part of the TNM system for pancreatic cancer:
Tumor (T)
Using the TNM system, the "T" plus a letter or number (0 to 4) is used to describe the size and location of the tumor. Tumor size is measured in centimeters (cm).
The tumor stage helps the doctor develop the best treatment plan for each patient. Specific tumor stage information is listed below.
TX: The primary tumor cannot be evaluated.
T0 (T zero): No evidence of cancer was found in the pancreas.
Tis: Refers to carcinoma in situ, which is very early cancer that has not spread.
T1: The tumor is in the pancreas only, and it is 2 cm or smaller in size. This stage may be further divided into T1a, T1b, and T1c based on the size of the tumor.
T2: The tumor is in the pancreas only, and it is larger than 2 cm but not larger than 4 cm.
T3: The tumor is larger than 4 cm and extends beyond the pancreas. It does not involve the major arteries or veins near the pancreas.
T4: The tumor extends beyond the pancreas into major arteries or veins near the pancreas. A T4 tumor cannot be completely removed with surgery.
Node (N)
The "N" in the TNM staging system is for lymph nodes. These small, bean-shaped organs located throughout the body help fight infection and disease as part of the body's immune system. In pancreatic cancer, regional lymph nodes are those lymph nodes near the pancreas, and distant lymph nodes are those lymph nodes in other parts of the body.
NX: The regional lymph nodes cannot be evaluated.
N0: Cancer was not found in the regional lymph nodes.
N1: Cancer has spread to 1 to 3 regional lymph nodes.
N2: Cancer has spread to 4 or more regional lymph nodes.
Metastasis (M)
The "M" in the TNM system describes whether the cancer has spread to other parts of the body, called metastasis.
M0: The disease has not spread to other parts of the body.
M1: Cancer has spread to another part of the body, including distant lymph nodes. Pancreatic cancer most commonly spreads to the liver, the lining of the abdominal cavity called the peritoneum, and the lungs.
Return to top
Stage groups for pancreatic cancer
Doctors assign the stage of the cancer by combining the T, N, and M classifications (see above).
Stage 0: Refers to cancer in situ, in which the cancer has not yet grown outside the duct in which it started (Tis, N0, M0).
Stage IA: The tumor is 2 cm or smaller in the pancreas. It has not spread to lymph nodes or other parts of the body (T1, N0, M0).
Stage IB: A tumor larger than 2 cm is in the pancreas. It has not spread to lymph nodes or other parts of the body (T2, N0, M0).
Stage IIA: The tumor is larger than 4 cm and extends beyond the pancreas. It has not spread to nearby arteries, veins, lymph nodes, or other parts of the body (T3, N0, M0).
Stage IIB: A tumor of any size has not spread to nearby arteries or veins. It has spread to 1 to 3 regional lymph nodes but not to other parts of the body (T1, T2, or T3; N1; M0).
Stage III: Either of these conditions:
- A tumor of any size that has spread to 4 or more regional lymph nodes but not to nearby arteries, veins, or other parts of the body (T1, T2, or T3, N2, M0).
- A tumor that has spread to nearby arteries and veins and may have spread to regional lymph nodes. It has not spread to other parts of the body (T4, any N, M0).
Stage IV: Any tumor that has spread to other parts of the body (any T, any N, M1).
Recurrent: Recurrent cancer is cancer that has come back after treatment. If the cancer does return, there will be another round of tests to learn about the extent of the recurrence. These tests and scans are often similar to those used during the original diagnosis .
Return to top
Used with permission of the American College of Surgeons, Chicago, Illinois. The original and primary source for this information is the AJCC Cancer Staging Manual, Eighth Edition (2017), published by Springer International Publishing.
Information about the cancer’s stage will help the doctor recommend a specific treatment plan. The next section in this guide is Types of Treatment . Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Types of Treatment
ON THIS PAGE: You will learn about the different types of treatments doctors use for people with pancreatic cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for pancreatic cancer. “Standard of care” means the best treatments known. These are the treatments that have been shown to be most effective based on evidence-based research conducted in clinical trials on a certain subset of patients. Information in this section is based on medical standards of care for pancreatic cancer in the United States. Treatment options can vary from one place to another.
When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials offer additional options to consider. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How pancreatic cancer is treated
In cancer care, different types of doctors who specialize in cancer, called oncologists, and other health care professionals often work together to create a patient’s overall care and treatment plan that combines different types of treatments and palliative and supportive care. This is called a multidisciplinary team. Cancer care teams include other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, patient navigators, social workers, pharmacists, counselors, dietitians, physical therapists, occupational therapists, and others. Learn more about the clinicians who provide cancer care.
Treatment options and recommendations depend on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of conversations are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is important for pancreatic cancer because there are different treatment options. Learn more about making treatment decisions .
When detected at an early stage, pancreatic cancer has a much higher chance of being successfully treated. However, there are also treatments that can help control the disease for patients with later stage pancreatic cancer to help them live longer and more comfortably.
The common types of treatments used for pancreatic cancer are described below, followed by a general outline of treatments by stage. Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
-
Surgery
-
Radiation therapy
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
-
Physical, emotional, social, and financial effects of cancer
-
Treatment options by stage of pancreatic cancer
-
Remission and the chance of recurrence
-
If treatment does not work
Surgery
Surgery for pancreatic cancer includes removing all or part of the pancreas, depending on the location and size of the tumor in the pancreas. An area of healthy tissue around the tumor is also often removed. This is called a margin. A goal of surgery is to have “clear margins” or “negative margins,” which means that there are no cancer cells in the edges of the healthy tissue removed. A surgical oncologist is a doctor who specializes in treating cancer using surgery.
About 20% of people diagnosed with pancreatic cancer are able to have surgery because most pancreatic cancers are found after the disease has already spread. When surgery is a potential treatment option, there are many things to think about before a surgery of this type. It's important to have a thorough discussion with your health care team, including a pancreatic surgical oncologist, before deciding on surgical treatment. This discussion should include talking about the benefits, risks, and recovery time of the specific surgery recommended for you. If surgery is not an option, you and your doctor will talk about other treatment options. It is common to seek a second opinion from a specialized surgical oncologist for less common cancers such as pancreatic cancer.
Surgery for pancreatic cancer may be combined with systemic therapy and/or radiation therapy (see below). Typically, these additional treatments are given after surgery, which is called adjuvant therapy. However, systemic therapy and/or radiation therapy may sometimes be used before surgery to shrink a tumor. This is called neoadjuvant therapy or pre-operative therapy. After neoadjuvant therapy, the tumor is re-staged before planning surgery. Re-staging is usually done with another computed tomography (CT) scan to look at the change in tumor size and what nearby structures and blood vessels it is affecting.
Different types of surgery are performed depending on the purpose of the surgery.
-
Laparoscopy. Sometimes, the surgeon may choose to start with a laparoscopy. During a laparoscopy, several small holes are made in the abdomen and a tiny camera is passed into the body while the patient receives anesthesia. Anesthesia is medication to help block the awareness of pain. During this surgery, the surgeon can find out if the cancer has spread to other parts of the abdomen. If it has, surgery to remove the primary tumor in the pancreas is generally not recommended.
-
Surgery to remove the tumor. Different types of surgery are used depending on where the tumor is located in the pancreas. In all of the surgeries discussed below, nearby lymph nodes are removed as part of the operation. More than 1 type of surgeon, as well as other specialists, will usually be involved in your surgery.
-
Whipple procedure. This surgery is also referred to as a pancreaticoduodenectomy. A Whipple procedure may be done if the cancer is located only in the head of the pancreas. This is an extensive surgery in which the surgeon removes the head of the pancreas and the part of the small intestine called the duodenum, as well as the bile duct and stomach, or sometimes just part of the stomach. Then, the surgeon reconnects the digestive tract and biliary system. Temporary drains are usually put in the abdomen to help it drain and assist with patient recovery. Drains are usually placed during surgery and remain in place after surgery to drain any leakage of pancreas juice to the outside of the body. Drains are left in place for a variable period based on the amount and nature of their output, but they can be removed while still in the hospital and can stay in place for up to 2 to 3 months. A surgeon with experience treating pancreatic cancer should perform this procedure. There are several variations of the Whipple procedure, such as standard, pylorus-preserving, and radical pancreaticoduodenectomy. Learn more about having this procedure in another article on this website.
-
Distal pancreatectomy. This surgery is commonly done if the cancer is located in the left side of the tail of the pancreas. In this surgery, the surgeon removes the tail and body of the pancreas, as well as the spleen.
-
Total pancreatectomy. If the cancer has spread throughout the pancreas or is located in many areas in the pancreas, a total pancreatectomy may be needed. A total pancreatectomy is the removal of the entire pancreas, part of the small intestine, a portion of the stomach, the common bile duct, the gallbladder, and the spleen.
-
Supportive surgery and palliative procedures are often recommended to help with symptoms impacting a patient’s quality of life. Examples of palliative procedures and surgery can include bypass surgery, stent placements, and nerve blocks to alleviate jaundice, nausea and vomiting, and tumor-associated pain.
After surgery, you will need to stay in the hospital. How long you will need to stay in the hospital for will be determined by the type of surgery you've had, but it can range from several days to several weeks or longer. It will also include an at-home rest and recovery plan. At-home rest could be for about a month or longer with full recovery expected to take about 2 months. Your health care team will work closely with you on your pre-surgery preparation plan and post-surgery recovery plan, including providing important exercise, drain management (when a drain is put in during surgery), mindfulness, and dietary and nutritional recommendations.
Side effects of surgery include weakness, tiredness, and pain for the first few weeks after the procedure. Other side effects caused by the removal of the pancreas sometimes include difficulty digesting food and diabetes from the loss of insulin produced by the pancreas. Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have and how they can be managed. For more information on relieving side effects, see the section entitled "Physical, emotional, social, and financial effects of cancer," below. Learn more about the basics of cancer surgery .
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. Learn more about the basics of radiation therapy .
External-beam radiation therapy is the type of radiation therapy used most often for pancreatic cancer. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. There are different ways that radiation therapy can be given:
-
Traditional radiation therapy. This is also called conventional or standard fraction radiation therapy. It is made up of daily treatments of lower doses of radiation per fraction or day. It is given over 5 to 6 weeks in total and is generally given during the week with weekends off from treatment.
-
Stereotactic body radiation (SBRT) or cyberknife. These are shorter treatments of higher doses of radiation therapy given over as few as 5 days. This is a newer type of radiation therapy that can provide more localized treatment in fewer treatment sessions. Whether this approach works as well as traditional radiation therapy is not yet known, and it may not be appropriate for every person. It should only be given in specialized centers that have experience and expertise in using this technology for pancreatic cancer and identifying who it will work best for.
-
Proton beam therapy. This is a type of external-beam radiation therapy that uses protons rather than x-rays. At high energy, protons can destroy cancer cells. This type of therapy also lessens the amount of healthy tissue that receives radiation. Proton beam therapy may be given for a standard amount of time or for a shorter time like SBRT. It is not yet known whether it works better than standard radiation therapy, and it may not be an option for every person. It should be given in treatment centers that have the experience and skills needed to use this treatment for pancreatic cancer, which may only be available through a clinical trial.
Other types of radiation therapy may also be offered. There are many different ways radiation therapy is given, so it's important to talk with your doctor about their planned approach.
Often, chemotherapy (see below) will be given at the same time as radiation therapy because it can enhance the effects of the radiation therapy, which is called radiosensitization. Combining chemotherapy and radiation therapy may occasionally help shrink the tumor enough so it can be removed by surgery. However, chemotherapy given at the same time as radiation therapy often has to be given at lower doses than when given alone.
Radiation therapy may be helpful for reducing the risk of the pancreatic cancer returning or re-growing in the original location. However, there remains much uncertainty as to how much, if at all, it lengthens a person’s life.
Side effects from radiation therapy may include fatigue, mild skin reactions, nausea, upset stomach, and loose bowel movements. Most side effects go away soon after treatment is finished. Talk with your health care team about what you can expect and how side effects will be managed.
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication. Medications are often given through an intravenous (IV) tube placed into a vein using a needle, or occasionally as a pill or capsule that is swallowed (orally). If you are given oral medications to take at home, be sure to ask your health care team about how to safely store and handle them and whether they may interact with any of your other medications.
Chemotherapy is the main type of systemic therapy used for pancreatic cancer. However, targeted therapy and immunotherapy are occasionally used and are being studied as potential treatments for certain individuals when test results show specific molecular or genetic features (see Latest Research ). Each of these types of therapies are discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases .
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. There is usually a rest period in between cycles. A patient may receive 1 drug at a time or a combination of different drugs given at the same time. The following drugs are approved by the U.S. Food and Drug Administration (FDA) for pancreatic cancer:
-
Capecitabine (Xeloda)
-
Fluorouracil (5-FU)
-
Gemcitabine (Gemzar)
-
Irinotecan (Camptosar)
-
Leucovorin (Wellcovorin)
-
Nab-paclitaxel (Abraxane)
-
Nanoliposomal irinotecan (Onivyde)
-
Oxaliplatin (Eloxatin)
Combination treatments are usually best for people who are able to carry out their usual activities of daily living without help. This is because there are generally more side effects when 2 or more drugs are used together.
The choice of which combination to use varies depending on a variety of factors about which is most appropriate for the patient, such as their specific diagnosis, stage of disease, treatment history, genetics, side effects, and overall health. For pancreatic cancer, chemotherapy may be described by when and how it is given:
-
First-line chemotherapy. This is generally the first treatment used for people with either locally advanced or metastatic pancreatic cancer who have not received prior treatment (see Stages ). The 2 most common first-line chemotherapy combinations used for pancreatic cancer are (1) FOLFIRINOX (5-FU, leucovorin, irinotecan, and oxaliplatin) and (2) gemcitabine plus nab-paclitaxel.
-
Second-line chemotherapy. If the first treatment does not work or stops working to control cancer growth, the cancer is called "refractory." Sometimes, first-line treatment does not work at all, which is called primary resistance. Or, treatment may work well for a while and then stop being effective later, which is sometimes called secondary or acquired resistance. In these situations, patients may benefit from additional treatment with different drugs if the patient’s overall health is good. There is significant ongoing research focused on developing other new treatments for second-line, as well as third-line, treatment and beyond. Some of these treatments have shown considerable promise (see the Latest Research section).
-
Off-label use. This refers to a drug being given for a condition not listed on its label . This means that the drug is not being given for the condition(s) that the drug is specifically approved for by the FDA. It can also mean that the drug is being given differently than the instructions on the label. An example of this is if a doctor wants to use a drug only approved for breast cancer to treat pancreatic cancer. Using a drug off-label is only recommended when there is solid evidence that the drug may work for another disease not included on the label. This evidence may include previously published research, promising results from ongoing research, or results from biomarker testing of the tumor that suggest the drug may work. However, off-label use of drugs may not be covered by your health insurance provider. Exceptions are possible, but it is important that you and/or your health care team talk with your insurance provider before this type of treatment begins.
Side effects of chemotherapy
The side effects of chemotherapy depend on which drugs you receive. In addition, not all patients have the same side effects even when given the same drug. Side effects in general can include poor appetite, nausea, vomiting, diarrhea, gastrointestinal problems, rash, mouth sores, hair loss, and a lack of energy. People receiving chemotherapy are also more likely to have low levels of white blood cells, red blood cells, and platelets, which give them a higher risk of anemia , infections, and bruising and bleeding easily.
Certain drugs used in pancreatic cancer are also linked with specific side effects. For example, capecitabine can cause redness and discomfort on the palms of the hands and the soles of the feet. This condition is called hand-foot syndrome . Both oxaliplatin and nab-paclitaxel can cause numbness and tingling in the fingers and toes, called peripheral neuropathy . Peripheral neuropathy is a side effect of nab-paclitaxel as well. These are examples, and it is important to talk with your doctor beforehand about side effects of the cancer medication(s) recommended for you.
Most side effects typically go away between treatments and after the treatments have ended, but some can be longer-lasting and can worsen as treatment continues. Your doctor can suggest ways to relieve these side effects . If the side effects are severe, your doctor may reduce the chemotherapy dose or pause chemotherapy for a short time.
Learn about the basics of chemotherapy .
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them.
-
Erlotinib (Tarceva). This drug is approved by the FDA for people with advanced pancreatic cancer in combination with the chemotherapy drug gemcitabine. Erlotinib blocks the effect of the epidermal growth factor receptor (EGFR), a protein that can become abnormal and help cancer grow and spread. This drug is taken as a pill orally by mouth, usually once a day. The side effects of erlotinib include a skin rash similar to acne , diarrhea, loss of appetite, and fatigue. This drug is not commonly used anymore due to its relatively modest benefit and the development of more effective therapies but is an option.
-
Olaparib (Lynparza). This drug is approved for people with metastatic pancreatic cancer associated with a germline (hereditary) BRCA mutation. It is intended for use as maintenance therapy after a patient has been on platinum-based chemotherapy, such as oxaliplatin or cisplatin, for at least 16 weeks with no evidence of disease progression. This drug is taken as a pill orally by mouth, usually twice a day. Common side effects from this drug can include nausea, vomiting, diarrhea or constipation, fatigue, feeling dizzy, loss of appetite, taste changes, low red blood cell counts, low white blood cell counts, belly pain, and muscle and joint pain.
-
Tumor-agnostic treatments. These refer to drugs that can be used for any type of cancer that has a specific genetic change, regardless of where the cancer started. These genetic changes tend to be rare in pancreatic cancer. When applicable, these drugs can be given to treat patients with pancreatic cancer that is metastatic or locally advanced that has not responded to chemotherapy. Examples of these drugs include:
-
Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek). These drugs are for tumors that have a particular genetic change called an NTRK fusion (see Diagnosis ). They are taken as pills orally by mouth. Common side effects can include dizziness, fatigue, nausea, vomiting, constipation, weight gain, and diarrhea.
-
Selpercatinib (Retevmo). This drug is used for tumors that have a RET fusion. Common side effects of this pill include fluid retention, diarrhea, fatigue, dry mouth, high blood pressure, abdominal pain, constipation, rash, nausea, and headache.
-
Dabrafenib plus trametinib. This combination of 2 different pills is used for tumors that have BRAF V600E mutations. Common side effects include fever, fatigue, nausea, rash, chills, headache, bleeding, cough, vomiting, constipation, diarrhea, muscle and joint aches, and fluid retention.
-
Other targeted therapies can sometimes be considered for off-label use (see above) if molecular testing of the tumor shows the presence of certain rare mutations or genetic changes that suggest possible benefit, such as sotarasib (Lumakras) or adagrasib (Krazati) for tumors with KRAS G12C mutations.
Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Learn more about the basics of targeted treatments .
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells.
Immune checkpoint inhibitors, which include anti-PD-1 antibodies such as pembrolizumab (Keytruda) and dostarlimab (Jemperli), are an option for treating pancreatic cancers that have high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), or high tumor mutational burden (TMB) (see Diagnosis ). Approximately 1% to 1.5% of pancreatic cancers are associated with high MSI-H.
Immunotherapy, combined with chemotherapy, is also being studied as part of emerging clinical trials.
Different types of immunotherapy can cause different side effects. Talk with your doctor about possible side effects of the immunotherapy recommended for you. Learn more about the basics of immunotherapy .
Return to top
Physical, emotional, social, and financial effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative and supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative and supportive care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative and supportive care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments, such as chemotherapy, surgery, or radiation therapy, to improve symptoms. Palliative and supportive care should not be confused with hospice care, which is used when a cure is not likely or when people are in the last months of life.
Before treatment begins, talk with your health care team about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative and supportive care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
Cancer care is often expensive, and navigating health insurance can be difficult. Ask your doctor or another member of your health care team about talking with a financial navigator or counselor who may be able to help with your financial concerns .
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of monitoring and tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Palliative and supportive care for people with pancreatic cancer may include:
-
Palliative chemotherapy. Any chemotherapy regimen discussed above may help relieve the symptoms of pancreatic cancer, such as lessening pain, improving a patient’s energy and appetite, and stopping or slowing weight loss. This approach is used when the cancer has spread and cannot be cured, but the symptoms of the cancer can be improved with chemotherapy. When making decisions about palliative chemotherapy, it is important that you and your doctor weigh the benefits with the possible side effects and consider how each treatment might affect your quality of life.
-
Relieving bile duct or small intestine blockage. If the tumor is blocking the common bile duct or small intestine, placing a tiny tube called a stent can help keep the blocked area open. This procedure can be performed using nonsurgical approaches, such as endoscopic retrograde cholangiopancreatography (ERCP), percutaneous transhepatic cholangiography (PTC), or endoscopy (see Diagnosis ). A stent can be either plastic or metal. The type used depends on the availability, insurance coverage/cost, a person’s expected lifespan, and whether the cancer will eventually be removed with surgery. In general, plastic stents are less expensive and are easier to insert and remove. However, they need to be replaced every few months, are associated with more infections, and are more likely to move out of place. Stents are typically placed inside the body, but sometimes, a tube may need to be placed through a hole in the skin of the abdomen to drain fluid, such as bile. This is called percutaneous drainage. Sometimes, a patient may need surgery to create a bypass and alleviate symptoms, even if the tumor itself cannot be completely removed.
-
Improving digestion and appetite. A special diet, medications, and specially prescribed enzymes may help a person digest food better if their pancreas is not working well or has been partially or entirely removed. Meeting with a dietitian/nutritionist is recommended for most patients, especially for those who are losing weight and have a poor appetite because of the disease. Daily exercise is highly recommended, and your doctor can work with you on an appropriate regimen.
-
Controlling diabetes. Insulin will usually be recommended if a person develops diabetes due to the loss of insulin produced by the pancreas, which is more common after a total pancreatectomy. Your health care team will help you with monitoring and controlling this condition.
-
Relieving pain and other side effects. Morphine-like drugs called opioid analgesics are often needed to help reduce pain. Special types of nerve blocks done by pain specialists may also be used. One type of nerve block is a celiac plexus block, which helps relieve abdominal or back pain. During a nerve block, the nerves are injected with either an anesthetic to stop pain for a short time or a medication that destroys the nerves and can relieve pain for a longer time. A nerve block can be performed either percutaneously (through the skin) or with an endoscopic ultrasound (see above). Depending on where the tumor is located, radiation therapy can sometimes be used to relieve pain. Learn more about managing pain .
Recommended palliative and supportive care may also include complementary therapies . It is important that you talk with your doctor before trying any complementary therapies to make sure they do not interfere with your other cancer treatments.
Palliative and supportive care is not limited to managing a patient’s physical symptoms. There may also also emotional issues, like anxiety or depression, and psychological issues that many patients experience that can be managed with professional help and support. A professional can help with developing coping skills and the overall difficulty of dealing with cancer. Cancer also affects caregivers and loved ones, and they are encouraged to seek out support as well.
Return to top
Treatment options by stage of pancreatic cancer
Different treatments may be recommended for each stage of pancreatic cancer. The general options by stage are described below. For more detailed descriptions, see “How pancreatic cancer is treated,” above. Your doctor will recommend a specific treatment plan for you based on your specific diagnosis and needs. Clinical trials may also be a treatment option for each stage.
Below are some of the possible treatments based on the stage of the cancer. The information below is based on American Society of Clinical Oncology (ASCO) guidelines for the treatment of pancreatic cancer. Your care plan may also include treatment for symptoms and side effects, an important part of pancreatic cancer care. Also, patients with any stage of pancreatic cancer are encouraged to consider clinical trials as a treatment option. Talk with your doctor about all of your treatment options. Your doctor will have the best information about which treatment plan is recommended for you.
Potentially curable pancreatic cancer (also called resectable and borderline resectable pancreatic cancer)
-
Surgery
-
Removal of the tumor and nearby lymph nodes if there are no signs that the disease has grown beyond the pancreas or spread to other parts of the body.
-
-
Treatment before surgery, also called neoadjuvant therapy or pre-operative therapy
-
Chemotherapy, with or without radiation therapy, is regularly used for patients with borderline resectable pancreatic cancer. It is done to try to shrink the tumor and increase the chance that the surgeon can remove the tumor with clear margins. Even for people with resectable pancreatic cancer, neoadjuvant therapy is also sometimes recommended.
-
-
Treatment after surgery, also called adjuvant therapy or post-operative therapy
-
Adjuvant chemotherapy usually starts within 4 to 12 weeks after surgery depending on how quickly a patient recovers. It is typically given for a total of 6 months. The type of combination chemotherapy given is usually FOLFIRINOX (5-FU, leucovorin, irinotecan, and oxaliplatin) for those patients who have recovered well from surgery and are healthy enough for a multidrug combination. The alternative option is gemcitabine, either as a single drug or in combination with a second drug called capecitabine. Multidrug combinations have been shown to be more effective than just gemcitabine alone, but are associated with more side effects , including diarrhea, fatigue, neuropathy, low levels of white blood cells, and hand-foot syndrome. Talk with your doctor about the best chemotherapy options for you.
-
The role of radiation therapy after surgery remains controversial. The option to use radiation therapy after surgery depends on each patient’s situation. For example, it may be an option for when there were not clear margins after surgery.
-
For patients who received treatment before surgery, the need for additional treatment after surgery depends on each patient’s situation and overall health.
-
Locally advanced pancreatic cancer
-
First-line therapy
-
Chemotherapy with a combination of drugs may be an option depending on each patient’s situation and overall health (see options listed under "Metastatic pancreatic cancer" below).
-
Radiation therapy may also be an option. It is used most often after chemotherapy when the cancer has not spread beyond the pancreas. The choice of the type of radiation therapy used, such as standard external beam or SBRT (see "Radiation therapy" above), depends on several factors, including the size and location of the tumor.
-
-
Second-line therapy
-
If the disease worsens during or after first-line treatment , options may include trying different chemotherapy. Or, it may be possible to use radiation therapy if the tumor has not spread beyond the pancreas and you have not already received it.
-
-
Clinical trials
-
If standard treatment options are not working, you may want to consider a clinical trial. Talk with your doctor about clinical trials that may be open to you.
-
Metastatic pancreatic cancer
If cancer spreads to another part in the body from where it started, it is referred to as metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials might also be an option, so talk with your doctor about clinical trials for which you may be eligible. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
Your treatment plan may include a combination of the treatments discussed above. Treatment options for people with metastatic pancreatic cancer depend heavily on a patient’s overall health, preferences, and support system.
Information below is based on the ASCO guideline, “ Metastatic Pancreatic Cancer .” Please note that this link takes you to another ASCO website.
Depending on factors such as your preferences, characteristics, and your comorbidity profile, first-line options include:
-
Chemotherapy with a combination of fluorouracil, leucovorin, irinotecan, and oxaliplatin, called FOLFIRINOX.
-
Gemcitabine plus nab-paclitaxel.
-
Gemcitabine by itself for patients who are not healthy enough for the more aggressive 2 combinations above.
-
Occasionally, another gemcitabine-based or fluorouracil-based combination may be used, such as gemcitabine plus cisplatin, gemcitabine plus capecitabine, or FOLFOX.
Second-line options include those listed below. These are generally for when the disease worsens or patients experienced severe side effects during first-line therapy.
-
Fluorouracil alone or combined with nanoliposomal irinotecan, irinotecan, or oxaliplatin may be recommended based on the overall health of the patient and shared decision-making.
-
Gemcitabine alone or in combination with nab-paclitaxel may be offered.
-
Pembrolizumab or dostarlimab is recommended when the cancer has high microsatellite instability (MSI-high) or mismatch repair deficiency (dMMR). It is important to note that only about 1 to 1.5% of people with pancreatic cancer have MSI-high disease. Patients whose tumors show high tumor mutational burden (TMB) are also candidates to receive pembrolizumab.
-
Certain oral targeted therapies can be used for patients whose tumors have rare genetic changes, including larotrectinib or entrectinib for cancers with an NTRK fusion; selpercatinib for cancers with a RET fusion; and the combination of dabrafenib plus trametinib for cancers with a BRAF V600E mutation.
-
Patients who have an inherited BRCA1 or BRCA2 mutation and who have received first-line platinum-based chemotherapy that stopped the cancer from growing or spreading for 16 weeks or more may continue treatment with chemotherapy or receive maintenance therapy with olaparib, a targeted therapy. Maintenance therapy is treatment with the goal of keeping the cancer in remission, and it is an option after shared decision-making between the patient and doctor.
Maintenance therapy can also be an option for patients whose disease has not progressed on first-line treatment, but who, due to side effects, may no longer be able to continue with their original treatment. The only approved maintenance therapy is olaparib, which is beneficial in people who have metastatic pancreatic cancer associated with a germline (hereditary) BRCA mutation following first-line platinum-based chemotherapy. For other patients, maintenance therapy might mean simplifying their original chemotherapy regimen. For example, it might be simplified from gemcitabine/nab-paclitaxel to gemcitabine alone, or from FOLFIRINOX to FOLFOX, FOLFIRI, or capecitabine. Learn more about the basics of maintenance therapy .
Palliative and supportive care will also be important to help relieve symptoms and side effects. Talk with your doctor as early as possible about the symptoms you are experiencing, your mental well-being, and the social support available to you. Treatment to ease any cancer-related pain or other symptoms will be offered.
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of your health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. It is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence .
If the cancer returns after the original treatment, it is called recurrent cancer. Pancreatic cancer may come back in or near the pancreas (called a local or regional recurrence), or elsewhere in the body (called a distant recurrence, which is similar to metastatic disease).
If a recurrence happens, a new cycle of diagnostic testing will begin to learn as much as possible about the extent and location of it. After this testing is done, you and your doctor will talk about the treatment options. The treatment of recurrent pancreatic cancer is similar to the treatments described above and usually involves chemotherapy. Radiation therapy or surgery may also be used to help relieve symptoms. Your doctor may suggest clinical trials that are studying new ways to treat recurrent pancreatic cancer. Whichever treatment plan you choose, palliative and supportive care will be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence .
Return to top
If treatment does not work
Recovery from pancreatic cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team and family and friends to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
Planning for your future care and putting your wishes in writing is important, especially at this stage of disease. Then, your health care team and loved ones will know what you want, even if you are unable to make these decisions. Learn more about putting your health care wishes in writing.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care, which is not the same as palliative and supportive care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with your doctor or a member of your palliative care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning .
After the death of a loved one, many people want and need support to help them cope with the loss. Learn more about grief and loss .
Return to top
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - About Clinical Trials
ON THIS PAGE: You will learn more about clinical trials, which are the main way that new medical approaches are studied to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to care for people with pancreatic cancer. To make scientific advances, doctors create research studies involving volunteers called clinical trials. Every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials.
Clinical trials are used for all types and stages of pancreatic cancer. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of treatments, new approaches to radiation therapy or surgery, and new methods of treatment.
People who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and the chance that the new treatment may not work. People are encouraged to talk with their health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment. Talk with your doctor about clinical trials for symptoms and side effects.
Deciding to join a clinical trial
People decide to participate in clinical trials for many reasons. For some, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the added uncertainty of a clinical trial in the hope of a better result. Others volunteer for clinical trials because they know that these studies are a way to contribute to the progress in treating pancreatic cancer. Even if they do not benefit directly from the clinical trial, their participation may benefit future people with pancreatic cancer.
Insurance coverage and the costs of clinical trials differ by location and by study. In some programs, some of the expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team and your insurance company first to learn if and how your treatment in a clinical trial will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, they may receive no treatment by being given a placebo or a “sugar pill.” When used, placebos are usually combined with standard treatment in most cancer clinical trials. Study participants will always be told when a placebo is used in a study. Find out more about placebos in cancer clinical trials .
Patient safety and informed consent
To join a clinical trial, people must participate in a process known as informed consent. During the informed consent process, a member of the health care team should provide a written or digital copy of the informed consent and:
-
Describe all of the treatment options so that the person understands how the new treatment differs from the standard treatment.
-
List all of the risks of the new treatment, which may or may not be different than the risks of standard treatment.
-
Explain what will be required of each person in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
-
Describe the purposes of the clinical trial and what researchers are trying to learn.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together. You will need to meet all of the eligibility criteria in order to participate in a clinical trial. Learn more about eligibility criteria in clinical trials.
People who participate in a clinical trial may stop participating at any time for personal or medical reasons. This may include that the new treatment is not working or there are serious side effects. Clinical trials are also closely monitored by experts who watch for any problems with each study. It is important that people participating in a clinical trial talk with their doctor and researchers about who will be providing their treatment and care during the clinical trial, after the clinical trial ends, and/or if they choose to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of cancer. For specific topics being studied for pancreatic cancer, learn more in the Latest Research section.
Cancer.Net offers more information about cancer clinical trials in other areas of the website, including a complete section on clinical trials .
There are many resources and services to help you search for clinical trials for pancreatic cancer, including the following services. Please note that these links will take you to separate, independent websites:
-
ClinicalTrials.gov. This U.S. government database lists publicly and privately supported clinical trials.
-
World Health Organization (WHO) International Clinical Trials Registry Platform. The WHO coordinates health matters within the United Nations. This search portal gathers clinical trial information from many countries’ registries.
Read more about the basics of clinical trials matching services .
In addition, you can find a free video-based educational program about cancer clinical trials located in another section of this website.
The next section in this guide is Latest Research . It explains areas of scientific research for pancreatic cancer. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Latest Research
ON THIS PAGE: You will read about the scientific research being done to learn more about pancreatic cancer and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about pancreatic cancer, ways to prevent it, how to best treat it, and how to provide the best care to people diagnosed with this disease. The following areas of research may include new options for patients through clinical trials. Always talk with your doctor about the best diagnostic and treatment options for you.
-
Early detection. The best chance of successful treatment is when pancreatic cancer is found early. This is why ongoing research is focused on finding and using special blood tests, diagnostic imaging tools, and other approaches to find pancreatic cancer at its earliest stages before it spreads. This includes finding it at precancerous stages, known as pancreatic intraepithelial neoplasia, or PanIN lesions. These screening approaches are typically being used for people who have a high risk for pancreatic cancer, such as those with a strong family history or a known genetic condition that increases the risk of pancreatic cancer. It is not yet known if these screening tools could be used effectively for the general population.
-
Genetic/molecular studies. In cancer, damaged or abnormal genes cause uncontrolled cell growth. Many new research developments are based on identifying damaged genes and proteins and repairing them or changing how they work.
Pancreatic tumor samples can be analyzed using a variety of molecular techniques, such as DNA sequencing and mutational analysis, to look for genetic changes. Some of these same analyses can now even also be performed on blood samples, as newer technologies allow for collection and analysis of tumor DNA present in the blood.
This information can then be used to develop new drugs that target these changes (see "Immunotherapy" and "Targeted therapy," below), as well as to potentially screen for pancreatic cancer in people who have a high risk of the disease. At this point, these tools are only being used in clinical trials.
-
Circulating tumor (ct)DNA. This refers to DNA that is shed by cancer cells into the bloodstream. It can now be detected and analyzed through a simple blood draw (or, less commonly, a urine sample) using current technologies. ctDNA is being studied as a tool for monitoring the tumor's response to treatment, for observing early signs of disease recurrence, and as a way to determine the disease's resistance to ongoing treatment.
-
Immunotherapy. As explained in the Types of Treatment section, cancer researchers are studying several types of immunotherapy as potential treatments for pancreatic cancer.
-
A number of clinical trials have been done or are ongoing that use cancer vaccines to try to treat a variety of types of cancer, including pancreatic cancer. Such vaccines may be made from various sources, including pancreatic cancer cells, bacteria, or a person’s specific tumor cells. Depending on the circumstances, vaccines may be given either after, during, or instead of chemotherapy.
-
Immune checkpoint inhibitors, such as anti-PD-1 antibodies, are already approved for other types of cancer, including melanoma and lung cancer. However, they are not yet approved for pancreatic cancer except for the few patients with tumors that have high microsatellite instability (see Types of Treatment ). Researchers are looking at other drugs that can harness a person's immune system in different ways. Ongoing studies in pancreatic cancer are testing the combination of different immunotherapies with each other or with chemotherapy, radiation therapy, or other targeted agents.
-
In addition, researchers are studying methods to collect and genetically modify a person’s T cells, which are a type of white blood cell. This is called adoptive immunotherapy. While this approach (such as chimeric antigen receptor therapy, or CAR T-cell therapy ) has advanced the way doctors treat some blood-based cancers such as leukemia and myeloma, researchers are still trying to learn how to apply it in solid tumors such as pancreatic cancer.
-
-
Targeted therapy. As discussed in the Types of Treatment section, the only targeted therapies currently approved for pancreatic cancer are erlotinib, which is no longer commonly used; olaparib, which is limited to pancreatic cancers associated with a germline (hereditary) BRCA mutation; and larotrectinib and entrectinib, which are limited to pancreatic cancers that harbor an NTRK fusion. Other drugs that may help block tumor growth and spread are being studied for pancreatic cancer, both as single drugs and as part of combination therapy. A gene called KRAS is often mutated in pancreatic cancer, and new drugs that target specific RAS mutations (in particular one called KRAS G12C that is present in about 2% of pancreatic cancers) show promising results. An additional strategy under evaluation entails inhibiting autophagy, a process used by cancer cells for self-protection by providing extra nutrients and keeping anticancer drugs from destroying them. Researchers are also studying drugs that can break down the stroma, which is the fibrous-like connective tissue that surrounds cancer cells and is involved in maintaining the cancer. By disrupting the tumor-associated stroma, these drugs may allow chemotherapy to reach and destroy cancer cells more effectively. Learn more about the basics of targeted therapy .
-
Gene therapy. Gene therapy is the delivery of specific genes to cancer cells, which are often carried by specially designed viruses. These include normal genes that are delivered into the center of cancer cells. Then, as the cancer cells divide, the working genes that were inserted in the cell replace the abnormal genes that contribute to cancer growth.
-
Chemotherapy. Newer, more effective types of standard chemotherapy continue to be researched.
-
Cancer stem cells. Pancreatic cancer stem cells are cells in the tumor that may be particularly resistant to standard therapies. Research is currently focused on identifying treatments that may specifically target those cancer stem cells.
-
Palliative and supportive care . Clinical trials are underway to find better ways of reducing symptoms and side effects of current pancreatic cancer treatments to improve comfort and quality of life for patients.
Looking for More About the Latest Research?
If you would like more information about the latest areas of research in pancreatic cancer, explore these related items that take you outside of this guide:
-
To find clinical trials specific to your diagnosis, talk with your doctor or search online clinical trial databases .
-
Visit the Cancer.Net Blog to review news and information about pancreatic cancer, including a study in advanced pancreatic cancer presented at the 2022 ASCO Annual Meeting .
-
Get updates from Cancer.Net delivered right to your inbox. Subscribe to the Inside Cancer.Net email newsletter.
-
Visit the website of Conquer Cancer, the ASCO Foundation , to find out how to help support cancer research. Please note that this link takes you to a different ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance on how to cope with the physical, emotional, social, and financial changes that cancer and its treatment can bring. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Coping with Treatment
ON THIS PAGE: You will learn more about coping with the physical, emotional, social, and financial effects of cancer and its treatment. Use the menu to see other pages.
Every cancer treatment can cause side effects or changes to your body and how you feel. For many reasons, people do not experience the same side effects even when they are given the same treatment for the same type of cancer. This can make it hard to predict how you will feel during treatment.
READ MORE BELOW:
-
Coping with physical side effects
-
Coping with emotional and social effects
-
Coping with the costs of cancer care
-
Coping with barriers to care
-
Talking with your health care team about side effects
-
Caring for a loved one with pancreatic cancer
As you prepare to start cancer treatment, it is normal to fear treatment-related side effects . It may help to know that your health care team will work to prevent and relieve side effects. This part of cancer treatment is called palliative and supportive care. It is an important part of your treatment plan, regardless of your age or the stage of disease.
Coping with physical side effects
Common physical side effects from each treatment option for pancreatic cancer are described in the Types of Treatment section. Learn more about side effects of cancer and its treatment, along with ways to prevent or control them . Changes to your physical health depend on several factors, including the cancer’s stage, the length and dose of treatment, and your general health.
Talk with your health care team regularly about how you are feeling. It is important to let them know about any new side effects or changes in existing side effects. If they know how you are feeling, they can find ways to relieve or manage your side effects to help you feel more comfortable and potentially keep any side effects from worsening. Staying as active as you are comfortable with and maintaining a healthy diet can all help your progress.
You may find it helpful to keep track of your side effects so it is easier to talk about any changes with your health care team. Learn more about why tracking side effects is helpful .
Sometimes, side effects can last after treatment ends. Doctors call these long-term side effects. Side effects that occur months or years after treatment are called late effects . Treating long-term side effects and late effects is an important part of survivorship care. Learn more by reading the Follow-Up Care section of this guide or talking with your doctor.
Return to top
Coping with emotional and social effects
You can have emotional and social effects after a cancer diagnosis. These may include dealing with a variety of emotions, such as sadness, anxiety, fear, or anger, or managing stress. Sometimes, people find it difficult to express how they feel to their loved ones. Some have found that talking to an oncology social worker, counselor, or member of the clergy can help them develop more effective ways of coping and talking about cancer. It is vital to have emotional support and to take care of your mental health needs during cancer. Remember that it is OK to ask for help and to let people know what your boundaries are.
You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your needs.
Return to top
Coping with the costs of cancer care
Cancer treatment can be expensive. It may be a source of stress and anxiety for people with cancer and their families. In addition to treatment costs, many people find they have extra, unplanned expenses related to their care. For some people, the high cost of medical care stops them from following or completing their cancer treatment plan. This can put their health at risk and may lead to higher costs in the future. Patients and their families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations in a separate part of this website.
Return to top
Coping with barriers to care
Some groups of people experience different rates of new cancer cases and experience different outcomes from their cancer diagnosis. These differences are called “cancer disparities.” Disparities are caused in part by real-world barriers to quality medical care and social determinants of health , such as where a person lives and whether they have access to food and health care. Cancer disparities more often negatively affect racial and ethnic minorities , people with fewer financial resources , sexual and gender minorities (LGBTQ+) , adolescent and young adult populations , adults older than 65 , and people who live in rural areas or other underserved communities .
If you are having difficulty getting the care you need, talk with a member of your health care team or explore other resources that help support medically underserved people .
Return to top
Talking with your health care team about side effects
Before starting treatment, talk with your doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they likely to happen?
-
What can we do to prevent or relieve them?
-
When and who should I call about side effects?
-
How long can these side effects last?
Be sure to tell your health care team about any side effects that happen during treatment and afterward, too. Tell them even if you do not think the side effects are serious. This discussion should include physical, emotional, social, and financial effects of cancer.
Return to top
Caring for a loved one with pancreatic cancer
Family members and friends often play an important role in taking care of a person with pancreatic cancer. This is called being a caregiver. Caregivers can provide physical, practical, and emotional support to the patient, even if they live far away. Being a caregiver can also be stressful and emotionally challenging. One of the most important tasks for caregivers is caring for themselves .
Caregivers may have a range of responsibilities on a daily or as-needed basis, including:
-
Providing support and encouragement
-
Talking with the health care team
-
Giving medications
-
Helping manage symptoms and side effects
-
Assisting with personal care and hygiene
-
Coordinating medical appointments
-
Providing a ride to and from appointments
-
Attending appointments with you to help take notes
-
Assisting with meals and grocery shopping
-
Helping with household chores
-
Handling insurance and billing issues
A caregiving plan can help caregivers stay organized and help identify opportunities to delegate tasks to others. It may be helpful to ask the health care team how much care will be needed at home and with daily tasks during and after treatment. Use this 1-page fact sheet to help make a caregiving action plan. This free fact sheet is available as a PDF, so it is easy to print.
Learn more about caregiving or read the ASCO Answers Guide to Caring for a Loved One With Cancer in English or Spanish .
Return to top
Looking for More on How to Track Side Effects?
Cancer.Net offers several resources to help you keep track of your symptoms and side effects. Please note that these links will take you to other sections of Cancer.Net:
-
Cancer.Net Mobile: The free Cancer.Net mobile app allows you to securely record the time and severity of symptoms and side effects.
-
ASCO Answers Fact Sheets: Read 1-page fact sheets on anxiety and depression , constipation , diarrhea , rash , and immunotherapy side effects that provide a tracking sheet to record details about the side effect. These free fact sheets are available as a PDF, so they are easy to print, fill out, and give to your health care team.
Return to top
The next section in this guide is Follow-Up Care . It explains the importance of check-ups after you finish cancer treatment. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Follow-Up Care
ON THIS PAGE: You will read about your medical care after cancer treatment is completed and why this follow-up care is important. Use the menu to see other pages.
Care for people diagnosed with pancreatic cancer does not end when active treatment has finished. Your health care team will continue to check that the cancer has not come back, manage any side effects, and monitor your overall health. This is called follow-up care.
Your follow-up care may include regular physical examinations and/or medical and imaging tests. Doctors want to keep track of your recovery in the months and years ahead. For people who have had surgery, follow-up visits every 3 to 6 months with the oncologist are typically recommended. Blood tests, including monitoring liver and kidney function and the tumor marker CA 19-9, may be done during these visits. For people with metastatic pancreatic cancer, a computed tomography (CT) scan or other imaging may also be used every 2 to 3 months after standard treatment begins to evaluate treatment effectiveness. The American Society of Clinical Oncology (ASCO) does not recommend the routine use of positron emission tomography (PET) scans for people with metastatic pancreatic cancer.
Cancer rehabilitation may be recommended, and this could mean any of a wide range of services, such as physical therapy, occupational therapy, career counseling, pain management, nutritional planning, and/or emotional counseling. The goal of rehabilitation is to help people regain control over many aspects of their lives and remain as independent as possible. Learn more about cancer rehabilitation.
Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence, which means that the cancer has come back. Cancer recurs because small areas of cancer cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms. During follow-up care, a doctor familiar with your medical history can give you personalized information about your risk of recurrence. Your doctor will ask specific questions about your health. Some people may have blood tests or imaging tests done as part of regular follow-up care, but testing recommendations depend on several factors, including the type and stage of cancer first diagnosed and the types of treatment given.
The anticipation before having a follow-up test or waiting for test results may add stress to you or a family member. This is sometimes called “scanxiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects
Most people expect to have side effects when receiving treatment. However, it is often surprising to survivors that some side effects may linger beyond the treatment period. These are called long-term side effects. Other side effects called late effects may develop months or even years after treatment has ended. Long-term and late effects can include both physical and emotional changes.
Talk with your doctor about your risk of developing such side effects based on your diagnosis, your individual treatment plan, and your overall health. If you had a treatment known to cause specific late effects, you may have certain physical examinations, scans, or blood tests to help find and manage them.
Keeping personal health records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health.
ASCO offers forms to help keep track of the cancer treatment you received and develop a survivorship care plan when treatment is completed. Many people choose to keep additional records of who they spoke with, the dates, and the tests, procedures, and results they received. You can also request copies of these records from your health care team throughout your diagnosis, treatment, and recovery. Or, you can request copies of the results of tests, procedures, and imaging scans at the time of or immediately after each test, procedure, or scan. Ask about getting copies of your medical records at the time the treatment or procedure is provided, as this helps save time in the event you need them later on for further consultation.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see their oncologist, while others transition back to the care of their primary care doctor or another health care professional. This decision depends on several factors, including the type and stage of cancer, side effects, health insurance rules, and your personal preferences.
If a doctor who was not directly involved in your cancer care will lead your follow-up care, be sure to share your cancer treatment summary and survivorship care plan forms with them and with all future health care providers. Details about your cancer treatment are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship . It describes how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Survivorship
ON THIS PAGE: You will read about how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to see other pages.
What is survivorship?
The word “survivorship” is complicated because it means different things to different people. Common definitions include:
-
Having no signs of cancer after finishing treatment.
-
Living with, through, and beyond cancer. According to this definition, cancer survivorship begins at diagnosis and continues during treatment and through the rest of a person’s life.
For some, the term “survivorship” itself does not feel right, and they may prefer to use different language to describe and define their experience. Sometimes long-term treatment will be used for months or years to manage or control cancer. Living with cancer indefinitely is not easy, and the health care team can help you manage the challenges that come with it . Everyone has to find their own path to name and navigate the changes and challenges that are the results of their cancer diagnosis and treatment.
Survivors may experience a mixture of feelings, including joy, concern, relief, guilt, and fear. Some people say they appreciate life more after a cancer diagnosis and have gained a greater acceptance of themselves. Others become very anxious about their health and uncertain about coping with everyday life. Feelings of fear and anxiety may still occur as time passes, but these emotions should not be a constant part of your daily life. If they persist, be sure to talk with a member of your health care team. It may help to keep a journal of your thoughts, as the act of writing them down often helps relieve some of the anxiety.
Survivors may feel some stress when their frequent visits to the health care team end after completing treatment. Often, relationships built with the cancer care team provide a sense of security during treatment, and people miss this source of support. This may be especially true when new worries and challenges surface over time, such as any late effects of treatment, emotional challenges including fear of recurrence, sexual health and fertility concerns, and financial and workplace issues.
Every survivor has individual concerns and challenges. With any challenge, a good first step is being able to recognize your fears and talk about them. Effective coping requires:
-
Understanding the challenge you are facing
-
Thinking through solutions
-
Asking for and allowing the support of others
-
Feeling comfortable with the course of action you choose
Many survivors find it helpful to join an in-person support group or an online community of survivors. This allows you to talk with people who have had similar first-hand experiences. Other options for finding support include talking with a friend or member of your health care team, individual counseling, or asking for assistance at the learning resource center of the place where you received treatment.
A new perspective on your health
For many people, survivorship serves as a strong motivator to make lifestyle changes.
People recovering from pancreatic cancer are encouraged to follow established guidelines for good health, such as not smoking, limiting alcohol, eating well, exercising regularly, and managing stress. Regular physical activity can help rebuild your strength and energy level. Your health care team can help you create an appropriate exercise plan based upon your needs, physical abilities, and fitness level. Learn more about making healthy lifestyle choices .
It is important to have recommended medical checkups and tests (see Follow-Up Care ) to take care of your health.
Talk with your health care team to develop a survivorship care plan that is best for your needs.
Changing role of caregivers
Family members and friends may also go through periods of transition. A caregiver plays a very important role in supporting a person diagnosed with cancer, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver's role often changes. Eventually, the need for caregiving related to the cancer diagnosis will become much less or come to an end. Caregivers can learn more about adjusting to life after caregiving .
Looking for More Survivorship Resources?
For more information about cancer survivorship, explore these related items. Please note that these links will take you to other sections of Cancer.Net:
-
ASCO Answers Guide to Cancer Survivorship: Get this 48-page booklet that helps people transition into life after treatment. It includes blank treatment summary and survivorship care plan forms. The free booklet is available as a PDF, so it is easy to print.
-
Survivorship Resources: Cancer.Net offers information and resources to help survivors cope, including specific sections for children , teens and young adults , and people over age 65 . There is also a main section on survivorship for people of all ages.
The next section offers Questions to Ask the Health Care Team to help start conversations with your cancer care team. Use the menu to choose a different section to read in this guide .
Pancreatic Cancer - Questions to Ask the Health Care Team
ON THIS PAGE: You will find some questions to ask your doctor or other members of the health care team to help you better understand your diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with the health care team is important to make informed decisions about your health care. These suggested questions are a starting point to help you learn more about your cancer care and treatment. You are also encouraged to ask additional questions that are important to you. As you think about the available time you have with your health care team, you will want to prioritize what questions are most important to you in the event there is not enough time to get to all your questions during an appointment. You may want to print this list and bring it to your next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your care. It may also be helpful to ask a family member or friend to come with you to appointments to help take notes. You may also want to keep a journal or notebook where you have all of your questions, notes, calendars, and other resources together.
Questions to ask after getting a diagnosis
-
What type of pancreatic cancer do I have?
-
Is my cancer located only in the pancreas?
-
What is the stage of the disease? What does this mean?
-
Can you explain my pathology report (laboratory test results) to me? Could I have a copy of the results?
-
Can you explain my imaging results to me? How can I get a copy of these results?
-
What is my prognosis (chance of recovery)?
-
Can my biopsy sample be used for genetic testing?
-
Can I donate tumor samples, blood samples, or body tissues to research for pancreatic cancer?
-
Is there a hereditary component to my cancer? Are my family members at increased risk?
Questions to ask about choosing a treatment and managing side effects
-
What are my treatment options?
-
What types of research are being done for pancreatic cancer in clinical trials? Do clinical trials offer additional treatment options for me?
-
What treatment plan do you recommend? Why?
-
What research studies support your recommendation for this treatment?
-
How do I understand in advance the costs of the recommended treatment?
-
What is the goal of each treatment? Is it to eliminate the cancer, help me feel better, or both?
-
Who will be part of my health care team, and what does each member do? Do they have experience treating pancreatic cancer?
-
Who will be leading my overall treatment?
-
What is the goal of each treatment?
-
What are the side effects of this treatment, both in the short term and the long term?
-
How will this treatment affect my daily life? Will I be able to work, exercise, and perform my usual activities?
-
Could this treatment affect my sex life? If so, how and for how long?
-
Could this treatment affect my ability to become pregnant or have children? If so, should I talk with a fertility specialist?
-
If I’m worried about managing the costs of cancer care, who can help me?
-
What support services are available to me? To my family?
-
If I have questions or problems, who should I call?
Questions to ask about having surgery
-
Is surgery a possibility to remove the cancer? If so, what type is recommended?
-
How experienced is my surgeon in performing this type of operation?
-
How often are there complications after this type of surgery, and what are the most common types of complications?
-
How long will the operation take?
-
What will I need to do to prepare for this surgery?
-
Will my surgery require a drain to be placed? How will the drain be monitored?
-
What type of anesthesia will I be given for this surgery?
-
What are the side effects of that anesthesia?
-
How long will I be in the hospital?
-
Can you describe what my recovery from surgery will be like?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having surgery?
-
If surgery is not a possibility, what are my other treatment options?
-
Can the surgeon use part of the tumor removed during surgery to conduct genetic tests on it?
-
How do I understand the possible out-of-pocket costs for my surgery and recovery?
-
Who will direct and oversee my follow-up care plan after surgery?
-
If I live far away from where my surgery took place, how will my care transition back to my local health care team?
Questions to ask about having radiation therapy
-
Should I receive radiation therapy? Why or why not?
-
What is the goal of this treatment?
-
What do I need to do to prepare for this treatment? Can I eat and drink beforehand?
-
How long will it take to give each treatment?
-
How many treatments will I receive?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
-
How will you evaluate the effects of the treatment on my tumor?
Questions to ask about having chemotherapy, targeted therapy, or immunotherapy
-
What is the goal of this treatment? Will this treatment help control the cancer?
-
How long will it take to give this treatment?
-
What do I need to do to prepare for this treatment?
-
Will I receive this treatment at a hospital or clinic? Or will I take it at home?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
-
What are the research studies that support this treatment? And how similar were the study participants to me in terms of their age, gender, ethnic background, and/or stage of disease?
Questions to ask about planning follow-up care
-
What is the chance that the cancer will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the cancer treatment I received?
-
What follow-up tests will I need, and how often will those tests be needed?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
When should I return to my primary care doctor for regular medical care?
-
Who will be leading my follow-up care?
-
What survivorship support services are available to me? To my family?
The next section in this guide is Additional Resources . It offers more resources on this website that may be helpful to you. Use the menu to choose a different section to read in this guide.
Pancreatic Cancer - Additional Resources
ON THIS PAGE: You will find some helpful links to other areas of Cancer.Net that provide information about cancer care and treatment. This is the final page of Cancer.Net’s Guide to Pancreatic Cancer. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of cancer for the person diagnosed and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Here are a few links to help you explore other parts of Cancer.Net:
-
Read more about the first steps to take when you are diagnosed with cancer .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of cancer care.
-
Learn more about coping with the emotions that cancer can bring, including those within a family or a relationship.
-
Find a national, not-for-profit advocacy organization that may offer additional information, services, and support for people with pancreatic cancer.
-
Explore what to do when you finish active treatment .
-
To find a range of information and insights from different voices on timely cancer topics, visit the Cancer.Net Blog .
-
Watch Cancer.Net videos with American Society of Clinical Oncology (ASCO) experts, patients, and caregivers explaining the basics of cancer treatment, side effects, survivorship, clinical trials, caregiving, and more.
-
For more information about treatment options for this disease, see the following topic review from UpToDate: Patient Information on Pancreatic Cancer (Beyond the Basics) . Please note that this link takes you to a separate, independent website.
This is the end of Cancer.Net’s Guide to Pancreatic Cancer. Use the menu to a different section to read in this guide.













