Meningioma - Introduction
ON THIS PAGE: You will find some basic information about this disease and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Meningioma. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
About the central nervous system
The brain and spinal column make up the central nervous system (CNS), which controls many of the vital functions of the body. When planning treatment for a tumor in the CNS , doctors consider how a person’s thought processes, movements, and senses may be affected by the tumor and potential treatment options.
About meningioma
A tumor begins when healthy cells change and grow out of control, often forming a mass. A tumor can be cancerous or benign. In general, a cancerous tumor is malignant, meaning it can spread or grow into other parts of the body. A benign tumor can grow but will usually not spread.
This guide focuses on meningioma. Meningioma is usually a slow-growing tumor that forms on the surface of the brain. It may cause significant symptoms if it grows and presses on the brain or spinal cord. Meningioma starts in the meningeal tissues, which are thin membranes that surround the brain and spinal cord. There are 3 meningeal layers: the dura mater, arachnoid, and pia mater. The meninges protect the brain and spinal cord and help the cerebrospinal fluid (CSF) circulate between the arachnoid and pia layers.
Around 80% of meningiomas are benign. The remaining 20% are either called atypical because they have an increased risk of returning after treatment or, rarely, malignant. Malignant meningioma may be called anaplastic.
Subtypes of meningioma
Meningioma is often classified based on where it starts in the CNS.
-
Falx and parasagittal meningioma. The falx is a membrane that sits in a groove between the left and right sides of the brain. It contains a large blood vessel and protects the brain. Parasagittal meningioma occurs at the top of the falx just on the inside of the skull. These are the most common types of meningioma and make up about 25% of all meningiomas.
-
Convexity meningioma. This type of meningioma occurs on the outer surface of the brain. It makes up about 20% of meningiomas.
-
Sphenoid meningioma. The sphenoidal ridge is located behind the eyes. This type makes up 20% of meningiomas.
-
Olfactory groove meningioma. This type of meningioma occurs near the nerves that connect the brain to the nose. It makes up 10% of meningiomas.
-
Posterior fossa meningioma. Posterior fossa meningioma develops at the back of the brain. It makes up 10% of all meningiomas.
-
Suprasellar meningioma. Suprasellar meningioma occurs next to the sella turcica. This is an area at the base of the skull in the center of the skull where the pituitary gland sits. This type makes up 10% of all meningiomas.
-
Spinal meningioma. Spinal meningioma usually occurs in the spine at chest level and may push against the spinal cord. It can cause pain radiating around the chest wall, bladder trouble, or weakness or numbness in the legs. This type makes up less than 10% of all meningiomas.
-
Intraorbital meningioma. This type of meningioma develops in or around the eye sockets. It accounts for less than 10% of meningiomas.
-
Intraventricular meningioma. Intraventricular meningioma occurs in the chambers that carry fluid throughout the brain. This type makes up about 2% of all meningiomas.
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
Cancer.Net Blog: Read an ASCO expert’s opinion on what newly diagnosed patients should know about a brain tumor.
-
Find a Cancer Doctor. Search for a specialist in your local area using this free database of doctors from the American Society of Clinical Oncology (ASCO).
-
Cancer Terms. Learn what medical phrases and terms used in tumor care and treatment mean.
The next section in this guide is Statistics . It helps explain the number of people who are diagnosed with meningioma and general survival rates. Use the menu to choose a different section to read in this guide.
Meningioma - Statistics
ON THIS PAGE: You will find information about the estimated number of people who will be diagnosed with meningioma each year. You will also read general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with a tumor are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this tumor and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for you individually. The original source for these statistics is provided at the bottom of this page.
How many people are diagnosed with meningioma?
A primary brain tumor is a tumor that begins in the brain. In the United States, meningioma accounts for 40% of primary brain tumors. In 2023, an estimated 42,260 people will be diagnosed with meningioma. Incidence rates of meningioma increase with age, with most cases diagnosed in adults age 65 and older. The disease is rarely found in children.
Women are diagnosed with meningioma more often than men. Black men and women are at a much higher risk for the disease than White men and women.
Most meningiomas are noncancerous. Malignant (cancerous) meningiomas are less common.
What is the survival rate for meningioma?
There are different types of statistics that can help doctors evaluate a person’s chance of recovery from meningioma. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having a tumor may affect life expectancy. Relative survival rate looks at how likely people with meningioma are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this tumor.
Example: Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) will be alive in 5 years.
It is important to remember that statistics on the survival rates for people with meningioma are only an estimate. They cannot tell an individual person if the tumor will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
The 5-year relative survival rate for malignant meningioma is 67%. The 10-year relative survival rate for malignant meningioma is 60%.
The survival rates for meningioma vary based on several factors. These include whether the tumor is cancerous, the stage and grade of the tumor, a person’s age and general health, and how well the treatment plan works.
The 5-year relative survival rate for malignant meningioma is 79% for children ages 0 to 14 and more than 84% in people ages 15 to 39. For adults 40 and over, the 5-year relative survival rate is around 65%.
For noncancerous meningioma, the 5-year relative survival rate is almost 97% for children ages 14 and under, 97% in people ages 15 to 39, and over 87% in adults 40 and older.
Experts measure relative survival rate statistics for meningioma every 5 years. This means the estimate may not reflect the results of advancements in how meningioma is diagnosed or treated from the last 5 years. Talk with your doctor if you have any questions about this information. Learn more about understanding statistics .
Statistics adapted from the Central Brain Tumor Registry of the United States Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2015–2019 ( published October 2022). (Source accessed February 2023.)
The next section in this guide is Medical Illustrations . It offers a drawing of the body parts often affected by meningioma. Use the menu to choose a different section to read in this guide.
Meningioma - Medical Illustrations
ON THIS PAGE: You will find a drawing about the main body parts affected by meningioma. Use the menu to see other pages.
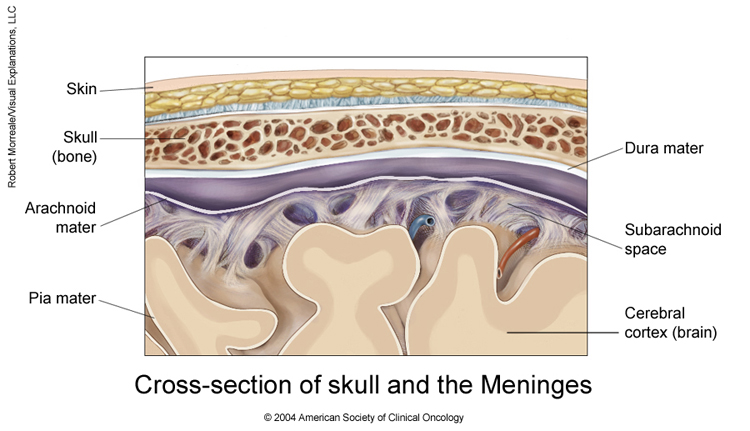
Copyright 2004 American Society of Clinical Oncology. Robert Morreale.
The next section in this guide is Risk Factors . It describes the factors that may increase the chance of developing meningioma. Use the menu to choose a different section to read in this guide.
Meningioma - Risk Factors
ON THIS PAGE : You will find out more about the factors that increase the chance of developing meningioma. Use the menu to see other pages.
What are the risk factors for meningioma?
A risk factor is anything that increases a person’s chance of developing a tumor. Although risk factors often influence the development of a tumor, most do not directly cause a tumor. Some people with several risk factors never develop meningioma, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor can help you make more informed lifestyle and health care choices.
The risk factors for meningioma include:
-
Age. Meningioma is most common in adults age 65 or older, but it can occur at any age. Meningioma is rare in children .
-
Sex. Women are about twice as likely as men to develop noncancerous meningioma. However, men and women are equally likely to be diagnosed with cancerous (malignant) meningioma.
-
Radiation exposure. Radiation to the head may increase a person’s risk of developing meningioma. Common sources of radiation that can cause meningioma include accidental exposure to radiation and radiation therapy as a treatment for ringworm on the scalp, called tinea capitis. Meningioma can also occur in people who have previously had radiation to the head as a treatment for another primary brain tumor like an astrocytoma, oligodendroglioma, or medulloblastoma.
-
Genetics. People with a hereditary syndrome called neurofibromatosis type 2 (NF2) have a higher risk of developing meningioma. People with NF2 are also more likely to develop cancerous meningioma or more than 1 meningioma.
-
Race/ethnicity. In the United States, Black people have higher rates of meningioma than White people. Meningioma is more common in Africa than in North America or Europe.
The next section in this guide is Symptoms and Signs . It explains what changes or medical problems meningioma can cause. Use the menu to choose a different section to read in this guide.
Meningioma - Symptoms and Signs
ON THIS PAGE: You will find out more about the changes and medical problems that can be a sign of meningioma. Use the menu to see other pages.
What are the symptoms and signs of meningioma?
People with meningioma may experience one or more of the following symptoms or signs. Symptoms are changes that you can feel in your body. Signs are changes in something measured, like taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. Sometimes, people with meningioma do not have any of the symptoms and signs described below. Or, the cause of a symptom or sign may be a medical condition that is not a tumor.
Symptoms of meningioma can be caused by the tumor pressing on the brain or spinal cord, stopping the normal functioning of a specific part of the brain, or pressing on nearby nerves or blood vessels. If the meningioma involves nearby bone, it may cause the bone to expand. Generally, meningioma is not diagnosed until symptoms begin.
General symptoms
General symptoms from the tumor pressing on the brain or spinal cord:
-
Seizures. Motor seizures, also called convulsions, are sudden involuntary movements of a person’s muscles. People may experience different types of seizures, including myoclonic, tonic-clonic (grand mal), sensory, and complex partial. Certain drugs can help prevent or control them. The differences between these types of seizures are explained below:
-
Myoclonic
-
Single or multiple muscle twitches, jerks, and/or spasms
-
Tonic-Clonic (Grand Mal)
-
Loss of consciousness and body tone, followed by twitching and relaxing muscle contractions
-
Loss of control of body functions
-
May be a short 30-second period of no breathing and the person may turn a shade of blue
-
After this type of seizure, a person may be sleepy and experience a headache, confusion, weakness, numbness, and sore muscles.
-
Sensory
-
Change in sensation, vision, smell, and/or hearing without losing consciousness
-
Complex partial
-
May cause a loss of awareness or a partial or total loss of consciousness
-
May be associated with repetitive, unintentional movements, such as twitching
-
Headaches, which may be severe and may worsen with activity or in the early morning
-
Personality or memory changes
-
Nausea or vomiting
-
Blurred vision
Symptoms specific to the tumor’s location
Symptoms of falx and parasagittal meningioma
-
Leg weakness
-
Headaches
-
Seizures
Symptoms of convexity meningioma
-
Seizures
-
Headaches
-
Focal neurological deficits. These are nerve problems that affect either a specific location or a small area. These problems may affect a side of the face or an arm or leg. They may also affect a smaller area like the tongue. The tumor can also affect a specific function. For example, speech may be affected but not the ability to write. It also may cause a loss of movement or feeling.
-
Personality or memory changes
Symptoms of sphenoid meningioma
-
Loss of feeling or numbness in the face
-
Loss of patches of sight within the field of vision, blindness, double vision
-
Headaches
Symptoms of olfactory groove meningioma
-
Loss of smell
-
Loss of patches of sight within the field of vision, blindness, double vision
-
Headaches
Symptoms of posterior fossa meningioma
-
Sharp pains in the face, facial numbness, and spasms of the facial muscles
-
Loss of hearing
-
Difficulty swallowing
-
Trouble walking
Symptoms of suprasellar meningioma
-
Swelling of the optic disk, which is in the retina of the eye where nerve fibers come together to form part of the optic nerve.
-
Loss of patches of sight within the field of vision, blindness, double vision
Symptoms of spinal meningioma
-
Back pain
-
Pain in the limbs or chest
-
Numbness and weakness or the arms and/or legs
-
Difficulties with bodily functions of the bowel or bladder
Symptoms of intraorbital meningioma
-
Bulging of the eye
-
Loss of vision
Symptoms of intraventricular meningioma
-
Personality or memory changes
-
Headaches
-
Dizziness
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will try to understand what is causing your symptom(s). They may do an exam and order tests to understand the cause of the problem, which is called a diagnosis.
If a brain tumor is diagnosed, relieving symptoms remains an important part of care and treatment. Managing symptoms may also be called "palliative and supportive care,” which is not the same as hospice care given at the end of life. This type of care focuses on managing symptoms and supporting people who face serious illnesses, such as cancer. You can receive palliative and supportive care at any time during treatment. Learn more in this guide’s section on Coping With Treatment .
Be sure to talk with your health care team about the symptoms you experience, including any new symptoms or a change in symptoms.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. Use the menu to choose a different section to read in this guide.
Meningioma - Diagnosis
ON THIS PAGE: You will find a list of common tests, procedures, and scans that doctors use to find the cause of a medical problem. Use the menu to see other pages.
Doctors use many tests to find, or diagnose, a tumor and learn if it is cancerous. They may also do tests to learn which treatments could work best.
For most tumor types, a biopsy or the removal of a tumor with surgery are the only sure ways for the doctor to know if an area of the body has a tumor. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis.
How meningioma is diagnosed
There are different tests used for diagnosing meningioma. Not all tests described here will be used for every person. Your doctor may consider these factors when choosing a diagnostic test:
-
The type of tumor suspected
-
Your signs and symptoms
-
Your age and general health
-
The results of earlier medical tests
Sometimes, meningioma is found accidentally while having a procedure for another reason. More commonly, meningioma is often diagnosed after a person starts having symptoms. A neuro-oncologist is a doctor who specializes in diagnosing and treating brain and nervous system tumors. The neuro-oncologist will use a patient’s symptoms as clues to the location of the tumor. In addition to a detailed medical history and physical examination, the following tests may help the doctor find and diagnose meningioma:
-
Neurological, vision, and hearing tests. These tests help find out how a possible tumor is affecting the brain. An eye examination can find changes to the optic nerve caused by pressure from a meningioma.
-
Stereotactic neurosurgery/biopsy. A biopsy can be performed during a procedure called a stereotactic technique. This technique uses a needle guided to the tumor with computers and imaging tests. A biopsy can also be done during surgery when the surgeon can look at the tumor directly. However, meningioma is usually removed rather than doing a separate biopsy. This means that surgery for meningioma is usually done by an open craniotomy instead of with stereotactic techniques. An open craniotomy is surgery where part of the skull is removed to provide access to the brain. The portion of skull removed during surgery is replaced after the tumor is removed. (More information on surgery can be found in the Types of Treatment section.)
-
Imaging tests. Sometimes, meningioma is diagnosed using only the imaging tests listed below because the location of the tumor may make a biopsy risky. Imaging tests show pictures of the inside of the body. Imaging tests are most useful when the results are combined with the patient’s medical history, physical examination, and neurological tests. This combination helps to more accurately find out where the tumor began and whether or where it has grown. The most common imaging tests used for diagnosing meningioma include:
-
Magnetic resonance imaging (MRI). An MRI produces detailed images of the inside of the body using magnetic fields, not x-rays. A special dye is injected into a patient’s vein before the scan to create a clearer picture. MRIs may create more detailed pictures than CT scans (see below) and often show changes in the brain caused by the tumor, such as swelling or areas where the tumor has grown. MRI is the preferred way to diagnose meningioma.
-
Computed tomography (CT or CAT) scan. A CT scan takes pictures of the brain by using x-rays of the head from many different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows any abnormalities or tumors. A CT scan can be used to measure the tumor’s size. Sometimes, a special dye called a contrast medium is injected into a patient’s vein before the scan to provide better detail on the image. A CT scan is best for finding changes in the skull that can be caused by meningioma. These changes may include the hardening of the area near the tumor, which can mean that the tumor has been there for a long time.
-
X-ray. A general x-ray creates a picture of the structures inside of the body using a small amount of radiation. An x-ray of the head can sometimes help doctors find out where a tumor is, but it is not enough to diagnose meningioma.
-
Cerebral angiogram. A cerebral angiogram shows the arteries in the brain. It is a special type of x-ray, or series of x-rays, of the head. X-rays are taken after a special dye called a contrast medium is injected into the main arteries of the head. Because meningioma can block important veins that drain blood from the brain, it is sometimes important to get an angiogram to plan surgery. In addition, there may be abnormal blood vessels that feed the tumor, and these can be seen with the angiogram. Sometimes, material is injected into the tumor before surgery to reduce bleeding during surgery.
After diagnostic tests are done, your doctor will review the results with you. If the diagnosis is meningioma, these results also help the doctor describe the tumor. This is called staging and grading.
The next section in this guide is Stages and Grades . It explains the system doctors use to describe the extent of the disease. Use the menu to choose a different section to read in this guide.
Meningioma - Stages and Grades
ON THIS PAGE: You will learn about how doctors describe meningioma and factors that help decide treatment options. This is called the stage and grade. Use the menu to see other pages.
READ MORE BELOW:
-
What is staging?
-
Determining treatment and prognosis for meningioma
-
Recurrent meningioma
-
Tumor markers
What is staging?
Staging is a way of describing where the tumor is located, if it is cancerous, if or where it has spread, and whether it is affecting other parts of the body. Doctors use diagnostic tests to find out the tumor’s stage, so staging may not be complete until all of the tests are finished. Knowing the stage helps the doctor recommend the best kind of treatment, and it can help predict a patient's prognosis, which is the chance of recovery. There are different stage descriptions for different types of tumors.
If meningioma has been diagnosed, additional tests will be done to learn more about the tumor. As described in Risk Factors , people with neurofibromatosis type 2 are more likely to have more than 1 meningioma. In this situation, a patient will have a variety of tests, including magnetic resonance imaging (MRI), to find out if or how much the tumor has spread within the brain and spine.
Return to top
Determining treatment and prognosis for meningioma
There is no formal staging system for meningioma because brain/spinal cord tumors cannot be staged the same way as tumors in other parts of the body. For meningioma, doctors use the 6 factors described below to determine the treatment options and prognosis:
Tumor histology and grade. As described in Diagnosis , a sample of the tumor is removed for analysis. Tumor histology includes the type of tumor, the grade, and additional molecular features that predict how quickly the tumor can grow. Together, these factors will help your doctor understand how the tumor will behave. These factors may also help determine a person’s treatment options .
Grade describes specific features in the tumor that are linked with specific outcomes. For example, doctors may consider whether the tumor cells are growing out of control or if there are a lot of dead cells. Tumors with features generally linked with growing more quickly are given a higher grade. For most tumors, the lower the grade, the better the prognosis.
In general, a meningioma is classified into 1 of 3 grades:
-
A grade I tumor grows slowly.
-
A grade II tumor grows more quickly and is often called atypical meningioma.
-
A grade III tumor grows and spreads very quickly and is often called anaplastic or malignant meningioma.
Age. In adults, the age that a person is diagnosed with meningioma is one of the best ways to predict prognosis. In general, the younger the person, the better the prognosis.
Extent of tumor residual. Resection is surgery to remove a tumor. Residual refers to how much of the tumor remains in the body after surgery. The prognosis is better when all of the tumor can be surgically removed. It includes 3 classifications:
-
Gross total. The entire tumor was removed, although microscopic cells may remain.
-
Subtotal. Large portions of the tumor were removed.
-
Biopsy only. Only a small portion, used for a biopsy, was removed.
Tumor location. Tumors can form in any part of the central nervous system (CNS). A tumor can cause more damage to some areas than others. Some tumors are harder to completely remove than others because of where they are located.
Functional neurologic status. The doctor will test how well a patient’s CNS is working by using one of several available assessment tools. One commonly used tool is called the Karnofsky Performance Scale . A higher score indicates a better prognosis.
Metastatic spread. Meningioma very rarely spreads to other parts of the body.
Return to top
Recurrent meningioma
A recurrent tumor is one that has come back after treatment. If the tumor returns, there will be another round of tests to learn about the extent of the recurrence. These tests and scans are often similar to those done at the time of the original diagnosis .
Return to top
Tumor markers
The factors described above are the best ways to determine the prognosis for a person with meningioma. Researchers are currently looking for tumor markers that could make meningioma easier to diagnose and allow the staging of adult CNS tumors. Tumor markers are substances found in higher-than-normal amounts in the blood, urine, or body tissues of people with certain tumor types. The goal is that someday it could be possible for doctors to use blood and/or other lab tests to help determine how quickly a brain tumor will grow and spread, develop more effective treatments, and more accurately predict prognosis.
Return to top
Used with permission of the American College of Surgeons, Chicago, Illinois. The original and primary source for this information is the AJCC Cancer Staging Manual, Eighth Edition (2017) , published by Springer International Publishing.
Information about the tumor will help the doctor recommend a specific treatment plan. The next section in this guide is Types of Treatment . Use the menu to choose a different section to read in this guide.
Meningioma - Types of Treatment
ON THIS PAGE: You will learn about the different types of treatments doctors use for people with meningioma. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for meningioma. “Standard of care” means the best treatments known. Information in this section is based on medical standards of care for meningioma in the United States. Treatment options can vary from one place to another.
When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials offer additional options to consider. A clinical trial is a research study that tests a new approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of meningioma. Your doctor can help you consider all your treatment options. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How meningioma is treated
Different types of doctors who specialize in tumors, called oncologists, often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team. For meningioma, this team may include neuro-oncologists, medical oncologists, neurologists, radiation oncologists, and surgeons. Medical care teams include other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, physical therapists, occupational therapists, and others. Learn more about the clinicians who provide medical care.
Meningioma is typically a slow-growing tumor. However, because a growing central nervous system (CNS) tumor can cause severe symptoms due to its location, people diagnosed with a CNS tumor should seek treatment as soon as possible. The pressure caused by a growing CNS tumor can cause serious symptoms that can damage delicate nerves and block cells from getting important nutrients.
Treatment options and recommendations depend on several factors, including the type and grade of the tumor, its location, possible side effects, and the patient’s preferences and overall health.
Treating brain and spinal cord tumors can be challenging. Surgery is the most common type of treatment, but it can be difficult if the tumor is near a delicate part of the brain or spinal cord. Radiation therapy is also commonly used. The blood-brain barrier, which normally protects the brain and spinal cord from damaging chemicals, also keeps out many types of chemotherapy. Meningioma grows outside the blood-brain barrier, so some drugs can reach these tumors. However, current chemotherapy options do not work very well for meningioma.
With continued research, more refined surgeries, a better understanding of the tumors that can be treated with chemotherapy, and precise delivery of radiation therapy have helped more patients with CNS tumors live longer and have a better quality of life.
Take time to learn about your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of conversations are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is important for meningioma because there are different treatment options.
Learn more about making treatment decisions .
The common types of treatments used for meningioma are described below, including surgery, radiation therapy, and very rarely, chemotherapy. Your care plan also includes treatment for symptoms and side effects, an important part of care for meningioma.
-
Active surveillance
-
Surgery
-
Radiation therapy
-
Chemotherapy
-
Physical, social, emotional, and financial effects
-
Remission and the chance of recurrence
-
If treatment does not work
Active surveillance
Because a grade I meningioma grows slowly, active surveillance may be recommended for some patients. This approach is also called watchful waiting or watch-and-wait. During active surveillance, the tumor is monitored and active treatment would begin if it started causing any symptoms or problems. This approach may be used for much older patients or for those with a tumor that was discovered accidentally and is not causing any symptoms. Often, patients continue to see their neurosurgeon for ongoing monitoring for a grade I meningioma. Talk with your doctor about any questions you may have, including whether this approach may be an option for you.
Return to top
Surgery
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. For meningioma, it is the most common treatment. And it is often the only treatment needed for a person with a noncancerous tumor that can be completely removed during surgery. For patients with a cancerous tumor or a tumor that cannot be fully removed during surgery, the treatment plan often includes radiation therapy and/or chemotherapy after surgery (see below).
Blocking the blood vessels that feed the tumor may be performed before surgery to reduce bleeding. Surgery to the brain is done by removing part of the skull, a procedure called a craniotomy. A neurosurgeon is a doctor who specializes in surgery of the brain and spinal cord. After the neurosurgeon removes the tumor, the patient’s own bone will be used to cover the opening in the skull.
In addition to removing or reducing the meningioma, surgery can be used to take a tumor sample for analysis under a microscope by a pathologist or neuropathologist (see Diagnosis ). A neuropathologist is a doctor who specializes in the diagnosis of diseases of the nervous system by studying tissue under a microscope. The results of the analysis can show if additional treatments, such as radiation therapy, will be necessary.
There have been rapid advances in surgery for brain tumors, including cortical mapping to identify the areas of the brain that control the senses, language, and motor skills and enhanced imaging methods to give surgeons more tools to plan and perform the surgery. Talk with your doctors to learn about the specific techniques that your surgery will include, including the possible side effects and what you can expect during your recovery.
Learn more about the basics of surgery .
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy tumor cells. A doctor who specializes in giving radiation therapy to treat a tumor is called a radiation oncologist. Doctors may recommend radiation therapy along with surgery to slow the growth of an aggressive tumor. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. Radiation therapy can be given in several ways.
Internal radiation therapy or brachytherapy is the use of tiny pellets or rods containing radioactive materials that are surgically implanted in or near the tumor. This approach is very rarely used for meningioma.
External-beam radiation therapy techniques use a machine outside the body to target the tumor. These techniques are becoming better able to direct radiation to the tumor while avoiding healthy tissue. For example, a linear accelerator is a special x-ray machine that moves around the body to direct pencil-thin beams of radiation to the brain tumor at different angles and intensities. This helps reduce the amount of healthy tissue exposed to radiation.
The following external-beam radiation therapy techniques may be used for meningioma:
-
Conventional radiation therapy. In this procedure, the direction of radiation is determined by features of the brain and skull and by x-rays. When a person’s entire brain needs to receive radiation therapy, this technique is appropriate. For more precise targeting, different techniques are needed.
-
Intensity modulated radiation therapy (IMRT). IMRT is a type of external-beam radiation therapy that can more directly target a tumor, further sparing healthy tissue from radiation therapy. In IMRT, the radiation beams are broken up into smaller beams and the intensity of each of these smaller beams can be changed. This means that the beams giving more radiation can be directed only at the tumor. IMRT is most useful to treat a tumor that is near critical parts of the brain, such as the brain stem and areas that control eyesight.
-
3-dimensional conformal radiation therapy. Based on computed tomography (CT) and magnetic resonance imaging (MRI) scans, a 3-dimensional model of the tumor and healthy tissues is created on a computer. Beam size and angles are determined that deliver more radiation to the tumor and less to the healthy tissue.
-
Stereotactic radiosurgery. Stereotactic radiosurgery delivers a single, high dose of radiation therapy directly to the tumor and not healthy tissue. It works best for a tumor that is only in 1 area of the brain and for some benign tumors, including most meningiomas. There are many different types of stereotactic radiosurgery equipment, including:
-
A modified linear accelerator, which is a machine that creates high-energy radiation by using electricity to form a stream of fast-moving particles that help kill tumor cells.
-
Gamma Knife is another form of radiation therapy that concentrates highly focused beams of gamma radiation on the tumor. A Gamma Knife can only be used for meningioma in the brain, not meningioma on the spine.
-
CyberKnife is a robotic device used in radiation therapy to guide the radiation to the tumor. It is most often used for tumors in the brain, head, and neck.
-
Fractionated stereotactic radiation therapy. Fractionated stereotactic radiation therapy is similar to stereotactic radiation therapy, except that it uses smaller, daily doses given over several days to several weeks. Precise positioning of the patient is very important, and a special head frame is used to target the radiation. This technique is best for tumors close to complex or sensitive structures, such as the optic (eye) nerves or brain stem.
-
Proton radiation therapy. Proton therapy is a type of external-beam radiation therapy that uses protons rather than x-rays. At high energy, protons can destroy tumor cells.
With these different techniques, doctors are trying to better target only the tumor and reduce the dose to the surrounding healthy tissue. Depending on the size and location of the meningioma, the radiation oncologist may choose any of the above radiation therapy techniques.
Learn more about the basics of radiation therapy .
Side effects of radiation therapy
Side effects from radiation therapy may include fatigue, mild skin reactions, hair loss, upset stomach, and neurologic symptoms. Most side effects go away soon after treatment is finished. Also, radiation therapy is usually not recommended for children younger than 5 because of the high risk of damaging their developing brains.
There are possible long-term side effects that may occur years after treatment. A person may experience cognitive problems, including memory loss and a slow decline in intellectual performance.
If the pituitary gland received radiation therapy, there may be changes in hormonal levels. The pituitary gland is a small gland near the brain that releases hormones that control bodily functions. In these situations, patients should be evaluated by an endocrinologist. An endocrinologist is a doctor who specializes in hormones, glands, and the endocrine system of the body.
How severe these side effects are depends on how much radiation therapy was given and where in the brain it was used. These side effects have become less severe with better technology and precision in radiation therapy. Talk with your radiation therapist before treatment begins if you have any questions or concerns about the possible long-term side effects of radiation therapy.
Return to top
Chemotherapy
Chemotherapy is the use of drugs to destroy tumor cells, usually by keeping the tumor cells from growing, dividing, and making more cells. Chemotherapy is given by a medical oncologist, a doctor who specializes in treating a tumor with medication, or a neuro-oncologist. Chemotherapy is rarely used to treat meningioma.
The side effects of chemotherapy depend on the individual and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away after treatment is finished.
Learn more about the basics of chemotherapy .
Return to top
Physical, emotional, social, and financial effects
Meningioma and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative and supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the tumor.
Palliative and supportive care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of tumor, may receive this type of care. And it often works best when it is started right after a diagnosis. People who receive palliative and supportive care along with treatment for the tumor often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative or supportive treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative or supportive treatments, such as chemotherapy, surgery, or radiation therapy, to improve symptoms. Common types of palliative and supportive care for people with a brain tumor include:
-
Steroids. Steroids occur naturally in the body in tiny amounts. In larger amounts, they are very powerful anti-inflammatory medications that reduce swelling. Most people with a brain tumor will need steroids to help relieve swelling of the brain. You will most likely receive steroids when you are first diagnosed, before and after surgery, before and after radiation therapy, and/or if you have an advanced brain tumor. Steroids may cause weight gain and water retention, increased appetite, difficulty sleeping, changes in mood, and stomach irritation. After successful treatment for the brain tumor, your doctor may slowly reduce the amount of steroids you need to take over time.
-
Anti-seizure medication. A person with a CNS tumor may experience seizures (see Symptoms and Signs ). This type of medication helps control how often a person has seizures.
-
Shunt. If fluid begins to build up in the brain, a surgeon may need to place a device called a shunt to bypass or move the fluid or drain the excess fluid.
-
Antidepressant medication. Depression can be common in people with a CNS tumor, but it is often undiagnosed. However, not all people with a CNS tumor experience depression. Let your health care team know how you are feeling on a regular basis. For those who have symptoms of depression, the health care team may decide to prescribe an antidepressant medication to help with your symptoms. Learn more about depression .
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative and supportive care options.
Medical care is often expensive, and navigating health insurance can be difficult. Ask your doctor or another member of your health care team about talking with a financial navigator or counselor who may be able to help with your financial concerns .
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Return to top
Remission and chance of recurrence
A remission is when the tumor cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the tumor will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the tumor returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the tumor does return. Learn more about coping with the fear of recurrence .
If the tumor returns after the original treatment, it is called a recurrent tumor. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence).
If a recurrence happens, a new cycle of testing will begin to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, radiation therapy, and chemotherapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent meningioma. Whichever treatment plan you choose, palliative and supportive care will be important for relieving symptoms and side effects.
The most common treatment for recurrent meningioma is additional surgery. If surgery cannot be done, radiation therapy is generally used. In addition, a patient can still receive care to manage the symptoms caused by the tumor. Symptom management is always important because the symptoms of meningioma can interfere with a person’s quality of life.
People with a recurrent tumor sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with a recurrence .
Return to top
If treatment does not work
Recovery from meningioma is not always possible. If the tumor cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced meningioma is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
Planning for your future care and putting your wishes in writing is important, especially at this stage of disease. Then, your health care team and loved ones will know what you want, even if you are unable to make these decisions. Learn more about putting your health care wishes in writing.
People who have advanced disease and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with your doctor or a member of your palliative care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced care planning .
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss .
Return to top
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for people with meningioma. Use the menu to choose a different section to read in this guide.
Meningioma - About Clinical Trials
ON THIS PAGE: You will learn more about clinical trials, which are the main way that new medical approaches are studied to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to care for people with meningioma. To make scientific advances, doctors create research studies involving volunteers, called clinical trials. Every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials.
Clinical trials are used for all types and stages of meningioma. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of treatments, new approaches to radiation therapy or surgery, and new methods of treatment.
People who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and the chance that the new treatment may not work. People are encouraged to talk with their health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment. Talk with your doctor about clinical trials for symptoms and side effects.
Deciding to join a clinical trial
People decide to participate in clinical trials for many reasons. For some, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the added uncertainty of a clinical trial in the hope of a better result. Others volunteer for clinical trials because they know that these studies are a way to contribute to progress in treating meningioma. Even if they do not benefit directly from the clinical trial, their participation may benefit future people with meningioma.
Insurance coverage and the costs of clinical trials differ by location and by study. In some programs, some of the expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team first to learn if and how your treatment in a clinical trial will be covered. You or your team may also need to contact your insurance company to find out what will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, they may receive no treatment by being given a placebo or a “sugar pill.” When used, placebos are usually combined with standard treatment in most cancer clinical trials. Study participants will always be told when a placebo is used in a study. Find out more about placebos in cancer clinical trials.
Patient safety and informed consent
To join a clinical trial, people must participate in a process known as informed consent. During informed consent, the doctor should:
-
Describe all of the treatment options, so that the person understands how the new treatment differs from the standard treatment.
-
List all of the risks of the new treatment, which may or may not be different from the risks of standard treatment.
-
Explain what will be required of each person in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
-
Describe the purposes of the clinical trial and what researchers are trying to learn.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together. You will need to meet all of the eligibility criteria in order to participate in a clinical trial. Learn more about eligibility criteria in clinical trials.
People who participate in a clinical trial may stop participating at any time for personal or medical reasons. This may include that the new treatment is not working or there are serious side effects. Clinical trials are also closely monitored by experts who watch for any problems with each study. It is important that people participating in a clinical trial talk with their doctor and researchers about who will be providing their treatment and care during the clinical trial, after the clinical trial ends, and/or if they choose to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of tumors. For specific topics being studied for meningioma, learn more in the Latest Research section.
Cancer.Net offers more information about clinical trials in other areas of the website, including a complete section on clinical trials .
There are many resources and services to help you search for clinical trials for meningioma, including the following services. Please note that these links will take you to separate, independent websites:
-
ClinicalTrials.gov. This U.S. government database lists publicly and privately supported clinical trials.
-
World Health Organization (WHO) International Clinical Trials Registry Platform. The WHO coordinates health matters within the United Nations. This search portal gathers clinical trial information from many countries’ registries.
Read more about the basics of clinical trials matching services .
In addition, you can find a free video-based educational program about cancer clinical trials in another section of this website.
The next section in this guide is Latest Research . It explains areas of scientific research for meningioma. Use the menu to choose a different section to read in this guide.
Meningioma - Latest Research
ON THIS PAGE: You will read about the scientific research being done to learn more about meningioma and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about meningioma, ways to prevent it, how to best treat it, and how to provide the best care to people diagnosed with this disease. The following areas of research may include new options for patients through clinical trials. Always talk with your doctor about the best diagnostic and treatment options for you.
-
Molecular drivers. Recent research has suggested that abnormalities, or mutations, in multiple genes may drive the formation of meningiomas. These genes include NF2 , TRAF7 , KLF4 , AKT1 , and SMO . There is ongoing research on how to target these genes for the treatment of meningiomas.
-
Hormonal drugs. Research has shown a possible link between meningioma and the body's hormone levels. Learn more about the basics of hormone therapy .
-
New treatments. Other new treatments that target the proteins that a tumor uses to grow are being studied in clinical trials. These types of treatments include the following:
-
Immunotherapy uses the body's natural defenses to fight a tumor by improving your immune system’s ability to attack tumor cells. Learn more about the basics of immunotherapy .
-
Drugs affecting other functions inside of tumor cells, including those that help tumor cells divide. Some of these are directed to specific pathways that may be unique or abnormally regulated compared with healthy cells. These types of treatments are called targeted therapy . Several studies for meningioma are examining this treatment approach.
-
Anti-angiogenesis therapy focuses on stopping angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to starve the tumor. Anti-angiogenesis therapy is a type of targeted therapy.
-
Gene therapy seeks to correct faulty genes that are causing tumor growth.
-
Directing electric fields through a portable device called the NovoTTF-100A (Optune) for cancerous meningioma.
-
Palliative and supportive care. Clinical trials are underway to find better ways of reducing symptoms and side effects of current meningioma treatments to improve comfort and quality of life for patients.
Looking for More About the Latest Research?
If you would like more information about the latest areas of research in brain tumors, explore these related items that take you outside of this guide:
-
To find clinical trials specific to your diagnosis, talk with your doctor or search online clinical trial databases .
-
Visit the Cancer.Net Blog to review news and information about brain tumors, including research announced at recent scientific meetings or in ASCO’s peer-reviewed journals.
-
Get updates from Cancer.Net delivered right to your inbox. Subscribe to the Inside Cancer.Net email newsletter.
-
Visit the website of Conquer Cancer, the ASCO Foundation , to find out how to help support cancer research. Please note that this link takes you to a different ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance on how to cope with the physical, emotional, social, and financial changes that meningioma and its treatment can bring. Use the menu to choose a different section to read in this guide.
Meningioma - Coping with Treatment
ON THIS PAGE: You will learn more about coping with the physical, emotional, social, and financial effects of meningioma and its treatment. Use the menu to see other pages.
Every treatment for meningioma can cause side effects or changes to your body and how you feel. For many reasons, people do not experience the same side effects even when they are given the same treatment. This can make it hard to predict how you will feel during treatment.
READ MORE BELOW:
-
Coping with physical side effects
-
Coping with emotional and social effects
-
Coping with the costs of medical care
-
Coping with barriers to care
-
Talking with your health care team about side effects
-
Caring for a loved one with meningioma
As you prepare to start treatment, it is normal to fear treatment-related side effects . It may help to know that your health care team will work to prevent and relieve side effects. This part of treatment is called palliative and supportive care. It is an important part of your treatment plan, regardless of your age or the stage of disease.
Coping with physical side effects
Common physical side effects from each treatment option for meningioma are described in the Types of Treatment section. Learn more about side effects of meningioma and its treatment, along with ways to prevent or control them . Changes to your physical health depend on several factors, including the tumor’s grade, the length and dose of treatment, and your general health.
Talk with your health care team regularly about how you are feeling. It is important to let them know about any new side effects or changes in existing side effects. If they know how you are feeling, they can find ways to relieve or manage your side effects to help you feel more comfortable and potentially keep any side effects from worsening.
You may find it helpful to keep track of your side effects so it is easier to talk about any changes with your health care team. Learn more about why tracking side effects is helpful .
Sometimes, side effects can last after treatment ends. Doctors call these long-term side effects. Side effects that occur months or years after treatment are called late effects . Treating long-term side effects and late effects is an important part of survivorship care. Learn more by reading the Follow-up Care section of this guide or talking with your doctor.
Return to top
Coping with emotional and social effects
You can have emotional and social effects after a diagnosis of meningioma. This may include dealing with a variety of emotions, such as sadness, anxiety, fear, or anger, or managing stress. Sometimes, people find it difficult to express how they feel to their loved ones. Some have found that talking to an oncology social worker, counselor, or member of the clergy can help them develop more effective ways of coping and talking about cancer.
You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your needs.
Return to top
Coping with the costs of medical care
Treatment for meningioma can be expensive. It may be a source of stress and anxiety for people with this diagnosis and their families. In addition to treatment costs, many people find they have extra, unplanned expenses related to their care. For some people, the high cost of medical care stops them from following or completing their treatment plan. This can put their health at risk and may lead to higher costs in the future. Patients and their families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations in a separate part of this website.
Return to top
Coping with barriers to care
Some groups of people experience different rates of new tumor cases and experience different outcomes from their diagnosis. These differences are called “health disparities.” Disparities are caused in part by real-world barriers to quality medical care and social determinants of health , such as where a person lives and whether they have access to food and health care. Health disparities more often negatively affect racial and ethnic minorities , people with fewer financial resources , sexual and gender minorities (LGBTQ+) , adolescent and young adult populations , adults older than 65 , and people who live in rural areas or other underserved communities .
If you are having difficulty getting the care you need, talk with a member of your health care team or explore other resources that help support medically underserved people .
Return to top
Talking with your health care team about side effects
Before starting treatment, talk with your doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they likely to happen?
-
What can we do to prevent or relieve them?
-
When and who should I call about side effects?
Be sure to tell your health care team about any side effects that happen during treatment and afterward, too. Tell them even if you do not think the side effects are serious. This discussion should include physical, emotional, social, and financial effects of meningioma.
Return to top
Caring for a loved one with meningioma
Family members and friends often play an important role in taking care of a person with meningioma. This is called being a caregiver. Caregivers can provide physical, practical, and emotional support to the patient, even if they live far away. Being a caregiver can also be stressful and emotionally challenging. One of the most important tasks for caregivers is caring for themselves .
Caregivers may have a range of responsibilities on a daily or as-needed basis, including:
-
Providing support and encouragement
-
Talking with the health care team
-
Giving medications
-
Helping manage symptoms and side effects
-
Coordinating medical appointments
-
Providing a ride to and from appointments
-
Assisting with meals
-
Helping with household chores
-
Handling insurance and billing issues
A caregiving plan can help caregivers stay organized and help identify opportunities to delegate tasks to others. It may be helpful to ask the health care team how much care will be needed at home and with daily tasks during and after treatment. Use this 1-page fact sheet to help make a caregiving action plan. This free fact sheet is available as a PDF, so it is easy to print.
Learn more about caregiving or read the ASCO Answers Guide to Caring for a Loved One With Cancer in English or Spanish .
Learn more about caring for a person with a brain tumor or metastatic brain cancer.
Return to top
Looking for More on How to Track Side Effects?
Cancer.Net offers several resources to help you keep track of your symptoms and side effects. Please note that these links will take you to other sections of Cancer.Net:
-
Cancer.Net Mobile: The free Cancer.Net mobile app allows you to securely record the time and severity of symptoms and side effects.
-
ASCO Answers Fact Sheets: Read 1-page fact sheets on anxiety and depression , constipation , diarrhea , and rash that provide a tracking sheet to record details about the side effect. These free fact sheets are available as a PDF, so they are easy to print, fill out, and give to your health care team.
Return to top
The next section in this guide is Follow-up Care . It explains the importance of checkups after treatment is finished. Use the menu to choose a different section to read in this guide.
Meningioma - Follow-Up Care
ON THIS PAGE: You will read about your medical care after treatment for meningioma is completed and why this follow-up care is important. Use the menu to see other pages.
Care for people diagnosed with meningioma does not end when active treatment has finished. Your health care team will continue to check that the tumor has not come back, manage any side effects, and monitor your overall health. This is called follow-up care.
Your follow-up care may include regular physical examinations, medical tests, or both. Doctors want to keep track of your recovery in the months and years ahead.
People treated for a benign meningioma typically have yearly follow-up visits with a neurosurgeon or neuro-oncologist. People with a more aggressive tumor may need checkups more often and ongoing medical care after recovery from surgery. People treated for either kind of meningioma will typically need regular, repeated magnetic resonance imaging (MRI) or computed tomography (CT) scans of the brain during their follow-up care, as well as physical examinations. If radiation therapy was given to the pituitary gland, evaluations of hormone levels may be needed. The frequency of the checkups and scans needed for follow-up care varies widely from patient to patient. Your follow-up care plan will be determined by your oncologist or neuro-oncologist.
Rehabilitation may be recommended, and this could mean any of a wide range of services, such as physical therapy, occupational therapy, career counseling, pain management, nutritional planning, and/or emotional counseling. The goal of rehabilitation is to help people regain control over many aspects of their lives and remain as independent as possible. Learn more about rehabilitation.
Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence, which means that the tumor has come back. Meningioma recurs because small areas of tumor cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms. During follow-up care, a doctor familiar with your medical history can give you personalized information about your risk of recurrence. Your doctor will ask specific questions about your health.
The anticipation before having a follow-up test or waiting for test results may add stress to you or a family member. This is sometimes called “scanxiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects
Most people expect to have side effects when receiving treatment. However, it is often surprising to survivors that some side effects may linger beyond the treatment period. These are called long-term side effects. Other side effects called late effects may develop months or even years after treatment has ended. Long-term and late effects can include both physical and emotional changes.
Meningioma and its treatments can affect the functioning of the brain as well as your daily well-being. For this reason, it is sometimes helpful for the health care team to monitor your quality of life and evaluate your cognitive (thought-process) abilities through specialized tests, often given by a neuropsychologist. A neuropsychologist is a psychologist who studies causes of brain disorders and specializes in diagnosing and treating these disorders using mostly a medical approach. These evaluations could identify certain problems that may benefit from specific therapies, such as speech therapy or occupational therapy , counseling with a social worker , or prescription medications that can help reduce fatigue or improve memory .
Talk with your doctor about your risk of developing such side effects based on your diagnosis, your individual treatment plan, and your overall health. If you had a treatment known to cause specific late effects, you may have certain physical examinations, scans, or blood tests to help find and manage them.
Keeping personal health records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. The American Society of Clinical Oncology (ASCO) offers forms to help keep track of the treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see their oncologist, while others transition back to the care of their primary care doctor or another health care professional. This decision depends on several factors, including the type and grade of meningioma, treatments received, side effects, health insurance rules, and your personal preferences.
If a doctor who was not directly involved in your care for meningioma will lead your follow-up care, be sure to share your treatment summary and survivorship care plan forms with them and with all future health care providers. Details about your treatment are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship . It describes how to cope with challenges in everyday life after a diagnosis of meningioma. Use the menu to choose a different section to read in this guide.
Meningioma - Survivorship
ON THIS PAGE: You will read about how to with challenges in everyday life after a diagnosis of meningioma. Use the menu to see other pages.
What is survivorship?
The word “survivorship” is complicated because it means different things to different people. Common definitions include:
-
Having no signs of the tumor after finishing treatment.
-
Living with, through, and beyond the diagnosis. According to this definition, survivorship begins at diagnosis and continues during treatment and through the rest of a person’s life.
For some, the term “survivorship” itself does not feel right, and they may prefer to use different language to describe and define their experience. Sometimes long-term treatment will be used for months or years to manage or control a tumor. Living with this diagnosis indefinitely is not easy, and the health care team can help you manage the challenges that come with it . Everyone has to find their own path to name and navigate the changes and challenges that are the results of their diagnosis and treatment.
Survivors may experience a mixture of feelings, including joy, concern, relief, guilt, and fear. Some people say they appreciate life more after the diagnosis and have gained a greater acceptance of themselves. Others become very anxious about their health and uncertain about coping with everyday life. Feelings of fear and anxiety may still occur as time passes, but these emotions should not be a constant part of your daily life. If they persist, be sure to talk with a member of your health care team.
Survivors may feel some stress when their frequent visits to the health care team end after completing treatment. Often, relationships built with the health care team provide a sense of security during treatment, and people miss this source of support. This may be especially true when new worries and challenges surface over time, such as any late effects of treatment, emotional challenges including fear of recurrence, sexual health and fertility concerns, and financial and workplace issues.
Every survivor has individual concerns and challenges. With any challenge, a good first step is being able to recognize your fears and talk about them. Effective coping requires:
-
Understanding the challenge you are facing
-
Thinking through solutions
-
Asking for and allowing the support of others
-
Feeling comfortable with the course of action you choose
Many survivors find it helpful to join an in-person support group or an online community of survivors. This allows you to talk with people who have had similar first-hand experiences. People with meningioma may find it more helpful to reach out to groups that provide support specifically for those with meningioma, rather than for all brain tumors.
Other options for finding support include talking with a friend or member of your health care team, individual counseling, or asking for assistance at the learning resource center of the place where you received treatment.
A new perspective on your health
For many people, survivorship serves as a strong motivator to make lifestyle changes.
People recovering from meningioma are encouraged to follow established guidelines for good health, such as not smoking, limiting alcohol, eating well, exercising regularly, and managing stress. Regular physical activity can help rebuild your strength and energy level. Your health care team can help you create an appropriate exercise plan based on your needs, physical abilities, and fitness level. Learn more about making healthy lifestyle choices .
It is important to have recommended medical checkups and tests (see Follow-up Care ) to take care of your health.
Talk with your health care team to develop a survivorship care plan that is best for your needs.
Changing role of caregivers
Family members and friends may also go through periods of transition. A caregiver plays a very important role in supporting a person diagnosed with meningioma, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver's role often changes. Eventually, the need for caregiving related to the diagnosis will become much less or come to an end. Caregivers can learn more about adjusting to life after caregiving .
Looking for More Survivorship Resources?
For more information about survivorship, explore these related items. Please note that these links will take you to other sections of Cancer.Net:
-
ASCO Answers Guide to Cancer Survivorship: Get this 48-page booklet that helps people transition into life after treatment. It includes blank treatment summary and survivorship care plan forms. This free booklet is available as a PDF, so it is easy to print.
-
Survivorship Resources: Cancer.Net offers information and resources to help survivors cope, including specific sections for children , teens and young adults , and people over age 65 . There is also a main section on survivorship for people of all ages.
The next section offers Questions to Ask the Health Care Team to help start conversations with your health care team. Use the menu to choose a different section to read in this guide.
Meningioma - Questions to Ask the Health Care Team
ON THIS PAGE: You will find some questions to ask your doctor or other members of the health care team, to help you better understand your diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with the health care team is important to make informed decisions about your health care. These suggested questions are a starting point to help you learn more about your care and treatment. You are also encouraged to ask additional questions that are important to you. You may want to print this list and bring it to your next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your care. It may also be helpful to ask a family member or friend to come with you to appointments to help take notes.
Questions to ask after getting a diagnosis
-
What type of meningioma do I have? Is it benign or cancerous?
-
What is the grade of the tumor? What does this mean?
-
How many patients with meningioma do you treat each year?
-
Do you attend expert meetings to discuss complicated tumor cases? What kinds of specialists attend such meetings?
-
Can you explain my pathology report (laboratory test results) to me?
-
Will an experienced neuropathologist review my pathology slides?
-
Is any special genetic testing needed? If so, can you describe this testing to me?
-
Do my family members have a higher risk of developing meningioma?
-
Do you have reading material that would help me understand this disease?
Questions to ask about choosing a treatment and managing side effects
-
What are my treatment options?
-
What types of research are being done for meningioma in clinical trials? Do clinical trials offer additional treatment options for me?
-
What treatment plan do you recommend? Why?
-
What is the goal of each treatment? Is it to eliminate the tumor, help me feel better, or both?
-
When should I start treatment?
-
Should I get a second opinion?
-
Where will my treatment take place? Are there brain tumor centers that you recommend?
-
Who will be part of my health care team, and what role does each person have?
-
Who will be leading my overall treatment?
-
What are the possible side effects of this treatment, both in the short term and the long term?
-
How will this treatment affect my daily life? Will I be able to work, exercise, drive, and perform my usual activities?
-
Could this treatment affect my sex life? If so, how and for how long?
-
Could this treatment affect my ability to become pregnant or have children? If so, should I talk with a fertility specialist before treatment begins?
-
If I’m worried about managing the costs of medical care, who can help me?
-
What support services are available to me? To my family?
-
Do you work with a social worker who assists patients with a brain tumor?
-
Do you know of a support group for patients with meningioma?
-
Who answers patient questions when you are unavailable?
-
If I have questions or problems, who should I call?
Questions to ask about having surgery
-
What type of surgery will I have?
-
How long will the operation take?
-
How long will I be in the hospital?
-
Can you describe what my recovery from surgery will be like?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term effects of having this surgery?
Questions to ask about having radiation therapy
-
What type of treatment is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about planning follow-up care
-
What is the chance that the tumor will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the treatment I received?
-
What follow-up tests will I need, and how often will those tests be needed?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
When should I return to my primary care doctor for regular medical care?
-
Who will be leading my follow-up care?
-
What survivorship support services are available to me? To my family?
The next section in this guide is Additional Resources . It offers more resources on this website that may be helpful to you. Use the menu to choose a different section to read in this guide.
Meningioma - Additional Resources
ON THIS PAGE: You will find some helpful links to other areas of Cancer.Net that provide information about cancer care and treatment. This is the final page of Cancer.Net’s Guide to Meningioma. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of a brain tumor for the person diagnosed and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Here are a few links to help you explore other parts of Cancer.Net:
-
Read more about the first steps to take when you are diagnosed with meningioma .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of medical care.
-
Learn more about coping with the emotions that a diagnosis of meningioma can bring, including those within a family or a relationship.
-
Find a national, not-for-profit advocacy organization that may offer additional information, services, and support for people with meningioma.
-
Explore what to do when you finish active treatment .
-
Download Cancer.Net Mobile , a free app that includes a symptom and side effect tracker, medication reminders, and other interactive resources.
-
To find a range of information and insights from different voices on timely topics, visit the Cancer.Net Blog .
-
Watch Cancer.Net videos with ASCO experts, patients, and caregivers explaining the basics of treatment, side effects, survivorship, clinical trials, caregiving, and more.
This is the end of the Cancer.Net’s Guide to Meningioma. Use the menu to choose a different section to read in this guide.













