Medulloblastoma - Childhood - Introduction
ON THIS PAGE: You will find some basic information about childhood medulloblastoma and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Childhood Medulloblastoma. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
About the central nervous system and brain tumors
The brain and spinal column make up the central nervous system (CNS), which is where all vital functions are controlled, including thought, speech, and body strength.
A brain tumor begins when healthy cells in the brain change and grow out of control, forming a mass. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but will not spread.
About medulloblastoma
Medulloblastoma is a type of brain tumor. Medulloblastoma begins in different cells in the cerebellum, which is the back of the brain. The cerebellum controls body movement and coordination.
Medulloblastoma occurs most commonly in children, and this section is about childhood medulloblastoma. It is the most common cancerous brain tumor in children. Learn more about other types of CNS tumors in children and brain tumors in adults .
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
Cancer.Net Patient Education Video: View a short video led by an American Society of Clinical Oncology (ASCO) expert in brain tumors that provides basic information and areas of research.
The next section in this guide is Statistics . It helps explain the number of children who are diagnosed with medulloblastoma and general survival rates. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Statistics
ON THIS PAGE: You will find information about the estimated number of children who will be diagnosed with medulloblastoma each year. You will also read general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with a tumor are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this tumor and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for your child individually. The original sources for these statistics are provided at the bottom of this page.
How many children are diagnosed with medulloblastoma?
About 500 children in the United States are diagnosed with medulloblastoma each year. About 20% of childhood brain tumors are medulloblastoma, making it the most common cancerous brain tumor in children.
The chance of developing medulloblastoma decreases with age. Most medulloblastomas occur in children between the ages of 1 and 9. Medulloblastoma can also occur in adults, but it is less common.
What is the survival rate for children with medulloblastoma?
There are different types of statistics that can help doctors evaluate a child’s chance of recovery from medulloblastoma. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having a tumor may affect life expectancy. Relative survival rate looks at how likely children with medulloblastoma are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this tumor.
Example: Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) to be alive in 5 years.
It is important to remember that statistics on the survival rates for children with medulloblastoma are only an estimate. They cannot tell an individual person if the tumor will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
The 5-year relative survival rate for medulloblastoma for children age 14 and younger is 72%. The 5-year relative survival rate for teens and young adults ages 15 to 39 is about 78%. The 5-year relative survival rate for people 40 or older is 66%.
The survival rates for children with medulloblastoma vary based on several factors. These include the stage of cancer, a person’s age and general health, and how well the treatment plan works. Another factor that can affect outcomes include the risk level for this disease. Learn more about risk level in the Stages section. Children who are younger than 3 may have a lower survival rate because not all safe and effective treatments can be used in this age group.
Experts measure relative survival rate statistics for medulloblastoma every 5 years. This means the estimate may not reflect the results of advancements in how medulloblastoma is diagnosed or treated from the last 5 years. Talk with your child’s doctor if you have any questions about this information. Learn more about understanding statistics .
Statistics adapted from the American Brain Tumor Association website, the Central Brain Tumor Registry of the United States Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2015–2019 (published October 2022), and the St. Jude Children’s Research Hospital website. (All sources accessed February 2023.)
The next section in this guide is Medical Illustrations . It offers a drawing of the part of the brain affected by medulloblastoma. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Medical Illustrations
ON THIS PAGE: You will find a drawing of the part of the brain affected by medulloblastoma. Use the menu to see other pages.
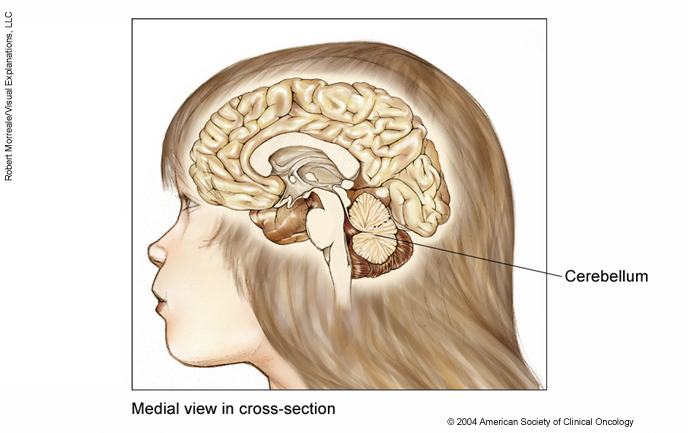
This illustration of the medial view of the brain in cross-section shows the cerebellum, located at the lower rear of the brain, behind and connected to the brain stem.
Copyright 2004 American Society of Clinical Oncology. Robert Morreale/Visual Explanations, LLC.
The next section in this guide is Risk Factors . It describes the factors that may increase the chance of developing medulloblastoma. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Risk Factors
ON THIS PAGE: You will find out more about the factors that increase the chance of developing childhood medulloblastoma. Use the menu to see other pages.
A risk factor is anything that increases a person’s chance of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause it. Some people with several risk factors never develop cancer, while others with no known risk factors do.
Doctors are gradually understanding what causes most childhood tumors, including medulloblastoma. The following factors are linked with a higher risk of medulloblastoma during childhood:
-
Gender. Medulloblastoma is more common in boys than in girls.
-
Age. Medulloblastoma occurs most often in the first 8 years of life, with about half of cases occurring in children younger than 6 years old.
-
Genetics. The following genetic conditions are associated with a higher risk of developing medulloblastoma:
-
Nevoid basal cell carcinoma syndrome (NBCCS)
-
Turcot syndrome, which is a subtype of familial adenomatous polyposis (FAP)
-
Lynch syndrome
-
BRCA1 gene mutations
-
The next section in this guide is Symptoms and Signs . It explains what changes or medical problems medulloblastoma can cause. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Symptoms and Signs
ON THIS PAGE: You will find out more about changes and other things that can signal a problem that may need medical care. Use the menu to see other pages.
Children with medulloblastoma may experience the following symptoms or signs. Symptoms are changes that you can feel in your body. Signs are changes in something measured, like by taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. Sometimes, children with medulloblastoma do not have any of the symptoms and signs described below. Or, the cause of a symptom or sign may be a medical condition that is not a brain tumor.
-
Headaches
-
Morning vomiting that worsens over time
-
Clumsiness
-
Problems with handwriting and other motor skills that worsen over time
-
Problems with vision or an eye turning inwards
If medulloblastoma spreads to the spinal cord, it may cause the following symptoms:
-
Back pain
-
Inability to control the bowels and bladder
-
Difficulty walking
If you are concerned about any changes your child experiences, please talk with your child’s doctor. Your child's doctor will ask how long and how often your child has been experiencing the symptom(s), in addition to other questions. This is to help figure out the cause of the problem, called a diagnosis .
If a brain tumor is diagnosed, relieving symptoms remains an important part of your child’s care and treatment. Managing symptoms may also be called "palliative care" or "supportive care." It is often started soon after diagnosis and continued throughout treatment. Be sure to talk with your child’s health care team about the symptoms your child experiences, including any new symptoms or a change in symptoms.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Diagnosis
ON THIS PAGE: You will find a list of common tests, procedures, and scans that doctors use to find the cause of a medical problem. Use the menu to see other pages.
Doctors use many tests to find, or diagnose, a brain tumor. They also do tests to learn if a cancerous tumor has spread to another part of the body from where it started. If the cancer has spread, it is called metastasis. Doctors may also do tests to learn which treatments could work best.
For most tumor types, a biopsy or surgery is the only sure way for the doctor to know if an area of the body has cancer. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy or surgery is not possible, the doctor may suggest other tests that will help make a diagnosis.
How medulloblastoma is diagnosed
There are many tests used for diagnosing medulloblastoma. Not all tests described here will be used for every child. Your child’s doctor may consider these factors when choosing a diagnostic test:
-
The type of tumor suspected
-
Your child’s signs and symptoms
-
Your child’s age and general health
-
The results of earlier medical tests
In addition to a physical examination, the following tests may be used to diagnose medulloblastoma:
-
Biopsy. A biopsy is the removal of a small amount of tissue for examination under a microscope. Other tests can suggest that a tumor is present, but looking at the tumor tissue removed during a biopsy, sometimes using surgery (see below), is the only way to make a definite diagnosis. A pathologist then analyzes the sample(s). A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease.
-
Surgical removal of the tumor . During surgery, a neurosurgeon removes as much of the tumor as possible (see the Types of Treatment section). A neurosurgeon is a doctor who specializes in removing a tumor from the brain or spine with surgery. A sample of the removed tissue is then examined under a microscope by a pathologist for a biopsy (see above).
-
Computed tomography (CT or CAT) scan. A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows any abnormalities or tumors. A CT scan can be used to measure the tumor’s size. Sometimes, a special dye called a contrast medium is given before the scan to provide better detail on the image. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow.
-
Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. MRI can be used to measure the tumor’s size. A special dye called a contrast medium is given before the scan to create a clearer picture. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow.
-
Lumbar puncture (spinal tap). A lumbar puncture is a procedure in which a needle is used to take a sample of cerebral spinal fluid (CSF) to look for cancer cells, blood, or tumor markers. Tumor markers are substances found in higher than normal amounts in the blood, urine, or body tissues of people with certain kinds of cancer. CSF is the fluid that flows around the brain and the spinal cord. The child is given an anesthetic that numbs the lower back before the procedure. For people with medulloblastoma, doctors usually perform a lumbar puncture after the tumor is removed through surgery (see the Types of Treatment section).
After diagnostic tests are done, your child’s doctor will review the results with you. If the diagnosis is medulloblastoma, these results also help the doctor describe the tumor. This is called staging.
The next section in this guide is Stages . It explains the system doctors use to describe the extent of the disease. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Stages
ON THIS PAGE: You will learn about how doctors describe this brain tumor’s growth or spread. This is called the stage. Use the menu to see other pages.
What is cancer staging?
Staging is a way of describing the size of a tumor, where it is located, if it is cancerous, if or where it has spread, and whether it is affecting other parts of the body.
Doctors use diagnostic tests to find out the tumor’s stage, so staging may not be complete until all of the tests are finished. Knowing the stage helps the doctor recommend the best kind of treatment and can help predict a patient’s prognosis, which is the chance of recovery. There are different stage descriptions for different types of tumors.
Medulloblastoma in children is classified as either standard (average) risk or high risk, depending on the following factors:
-
The child’s age
-
How much of the tumor remains after surgery
-
Whether the tumor has spread
Standard-risk tumor
The tumor is in the very back part of the brain and has not spread to other areas of the brain and spinal cord. Additionally, it is almost completely removed during surgery, meaning that less than 1.5 cubic centimeters (cm) of the tumor remains after surgery. However, the surgeon will usually prefer to remove all of the tumor if it can be completely removed without increasing the risk of severe side effects. Standard-risk tumors do not have molecular features that are linked with a worse chance of recovery.
High-risk tumor
Medulloblastoma has either spread to other parts of the brain or the spine, or it has not spread but more than 1.5 cubic cm of tumor remains after surgery. Some tumors that first appear to be standard-risk tumors will be found to have high-risk molecular features after testing is finished. In that case, the classification will change, and it will be treated as a high-risk tumor with the current standard treatment plans (see the Types of Treatment section).
Recurrent tumor
A recurrent tumor is a tumor that has come back after treatment. Medulloblastoma may recur in the brain, spine, spinal fluid, or, very rarely, elsewhere in the body. If the tumor does return, there will be another round of tests to learn about the extent of the recurrence. These tests and scans are often similar to those done at the time of the original diagnosis .
Information about the tumor’s risk classification will help the doctor recommend a specific treatment plan. The next section in this guide is Types of Treatment . Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Types of Treatment
ON THIS PAGE: You will learn about the different treatments doctors use for children with medulloblastoma. Use the menu to see other pages.
In general, brain tumors in children are uncommon. This means it can be hard for doctors to plan treatment unless they know what has been most effective in other children. That is why more than 60% of children with cancer are treated as part of a clinical trial. A clinical trial is a research study that tests a new approach to treatment. The “standard of care” is the best treatments known based on previous clinical trials. Clinical trials may test such approaches as a new drug, a new combination of existing treatments, or new doses of current therapies. The health and safety of all children participating in clinical trials are closely monitored.
To take advantage of these newer treatments, children with a brain tumor should be treated at a specialized medical center. Doctors at these centers have extensive experience in treating children and have access to the latest research. A doctor who specializes in treating children with cancer is called a pediatric oncologist. If a pediatric cancer center is not nearby, general cancer centers sometimes have pediatric specialists who are able to be part of your child’s care.
How medulloblastoma is treated
In many cases, a team of doctors works with a child and the family to provide care. This is called a multidisciplinary team . Pediatric cancer centers often have extra support services for children and their families, such as child life specialists, dietitians, physical and occupational therapists, social workers, and counselors. Special activities and programs to help your child and family cope may also be available.
Treatment options and recommendations depend on several factors, including the type and stage of the tumor, possible side effects, the family's preferences, and your child's overall health. Take time to learn about your child’s treatment options and be sure to ask questions about things that are unclear. Talk with your child’s doctor about the goals of each treatment and what your child can expect while receiving the treatment. These types of talks are called "shared decision-making." Shared decision-making is when you and your child's doctors work together to choose treatments that fit the goals of your child's care. Shared decision-making is particularly important for medulloblastoma because there are different treatment options. Learn more about making treatment decisions .
The main types of treatment used to treat medulloblastoma include surgery, radiation therapy, and chemotherapy. Current treatment plans tailor treatment recommendations based on the molecular subgroup of medulloblastoma (see
Latest Research
). Sometimes, the treatments are used in combination. In some situations, stem cell or bone marrow transplantation may be recommended.
Each of these common treatments is described below. Your child’s care plan also includes treatment for symptoms and side effects, an important part of medical care.
-
Surgery
-
Radiation therapy
-
Chemotherapy
-
Bone marrow transplantation/stem cell transplantation
-
Physical, emotional, and social effects of medulloblastoma
-
Remission and the chance of recurrence
-
If treatment does not work
Surgery
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. Most commonly, it is the first treatment used for medulloblastoma. In addition to removing or reducing the size of the tumor, surgery can provide a tissue sample to diagnose the tumor (see the Diagnosis section).
Surgery to the brain requires the removal of part of the skull, a procedure called a craniotomy. After the surgeon removes the tumor, the patient’s own bone will be used to cover the opening in the skull. There have been rapid advances in surgery for brain tumors. This includes the use of enhanced imaging machines to give surgeons more tools to plan and perform the surgery and cortical mapping. Cortical mapping is a technique that allows doctors to identify certain areas of the brain that control the senses, language, and motor skills.
With cancerous tumors, even if the cancer cannot be cured, removing it can provide significant relief of symptoms that are caused by the tumor pressing on the brain.
Some brain tumors cannot be removed by surgery because of their location. These tumors are called inoperable. In these situations, the doctor will recommend other treatment options.
Side effects from surgery for medulloblastoma can vary. Occasionally, the surgeon will place a plastic tube called a shunt to move the fluid made inside the brain to the abdomen so that the fluid does not build up in the brain and cause problems. In most instances, the placement of a shunt is safe, and most children do not have any problems from the procedure.
Before surgery, talk with your child's health care team about the possible side effects from the specific surgery your child will have. Learn more about the basics of surgery .
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy tumor cells. A doctor who specializes in giving radiation therapy is called a radiation oncologist. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. When radiation treatment is given using implants, it is called internal radiation therapy or brachytherapy. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
One type of radiation therapy that may be used for medulloblastoma is proton therapy. Proton therapy is a type of external-beam radiation therapy that uses protons rather than x-rays. At high energy, protons can destroy tumor cells. Talk with your child's doctor about whether proton therapy is recommended and available nearby.
Because radiation therapy can sometimes interfere with the growth and development of a child’s brain and spine, the doctor may choose to treat the tumor in another way. If radiation therapy is recommended, the approach will be based on the child’s age and the features of the tumor (see Stages ):
-
For children older than 3, radiation therapy is given to the entire brain and spine, followed by radiation therapy aimed directly at the tumor and the surrounding area or the back part of the brain.
-
For children younger than 3, radiation therapy may be directed only to the back part of the brain or the tumor and the surrounding area after surgery and chemotherapy (see below).
Short-term side effects from radiation therapy may include fatigue, mild skin reactions, vomiting, and loss of appetite. Most of these side effects go away soon after treatment is finished. Long-term side effects of radiation therapy may include problems with growth, low hormone levels, and problems with learning, especially higher education. Talk with your child's health care team beforehand about possible side effects and how they can be avoided or managed.
Learn more about the basics of radiation therapy .
Return to top
Chemotherapy
Chemotherapy is the use of drugs to destroy tumor cells, usually by keeping the tumor cells from growing, dividing, and making more cells.
Chemotherapy may be given by an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). It can also be given by injection into a muscle or directly into the cerebrospinal fluid (CSF). CSF is fluid that circulates around the brain and spinal cord.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or a combination of different drugs given at the same time.
Researchers are studying ways to use chemotherapy before, during, or after radiation therapy, as the 2 types of treatment may work better to treat medulloblastoma when combined.
Chemotherapy given in higher doses works best when there is little tumor left after surgery. When and how chemotherapy may be used is based on the child’s age:
-
High-dose chemotherapy may be used before or instead of radiation therapy for children younger than 3 to 4 years old.
-
Several cycles of chemotherapy may be used after radiation therapy in children older than 3 to 4 years old.
The side effects of chemotherapy depend on the individual and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away after treatment is finished.
The medications used to treat medulloblastoma are continually being evaluated. Talking with your child’s doctor is often the best way to learn about the medications prescribed for your child, their purpose, and their potential side effects or interactions with other medications. It is also important to let your doctor know if your child is taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with medications to treat the tumor, causing unwanted side effects or reduced effectiveness. Learn more about your child’s prescriptions by using
searchable drug databases
.
Learn more about the basics of chemotherapy .
Return to top
Bone marrow transplantation/stem cell transplantation
A bone marrow transplant may be used for children with recurrent medulloblastoma, which is when the tumor returns after treatment (see below). A bone marrow transplant is a medical procedure in which bone marrow that contains tumor cells is replaced by highly specialized cells. These cells, called hematopoietic stem cells, develop into healthy bone marrow. Hematopoietic stem cells are blood-forming cells found both in the bloodstream and in the bone marrow. This procedure is also called a stem cell transplant or a hematopoietic stem cell transplant.
Before recommending transplantation, doctors will talk with you about the risks of this treatment. They will also consider several other factors, such as the type of tumor, results of any previous treatment, and your child’s age and general health.
There are 2 types of hematopoietic stem cell transplantation depending on the source of the replacement blood stem cells: allogeneic (ALLO) and autologous (AUTO). ALLO uses donated stem cells, while AUTO uses the patient’s own stem cells. In both types, the goal is to destroy all of the tumor cells in the bone marrow, blood, and other parts of the body using high doses of chemotherapy and/or radiation therapy and then allow replacement blood stem cells to create healthy bone marrow.
Only AUTO transplantation is commonly used to treat medulloblastoma. ALLO transplantation is rarely recommended for children with medulloblastoma.
Side effects depend on the type of transplant, your child’s general health, and other factors. Learn more about the basics of bone marrow transplantation and stem cell transplantation .
Return to top
Physical, emotional, and social effects of medulloblastoma
Medulloblastoma and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your child’s care that is included along with treatments intended to slow, stop, or eliminate the tumor.
Supportive care focuses on improving how your child feels during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of disease, may receive this type of care. And it often works best when it is started right after a diagnosis. People who receive symptom management along with treatment for the tumor often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Supportive care techniques vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies.
Before treatment begins, talk with your child’s doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and supportive care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your child’s health care team may ask you to answer questions about your child’s symptoms and side effects and to describe each problem. Be sure to tell the health care team if your child is experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative and supportive care in a separate section of this website.
Return to top
Remission and the chance of recurrence
A remission is when medulloblastoma cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the tumor will come back. While many remissions are permanent, it is important to talk with your child’s doctor about the possibility of the tumor returning. Understanding your child’s risk of recurrence and the treatment options may help you feel more prepared if the disease does return. Learn more about coping with the fear of recurrence .
If medulloblastoma returns after the original treatment, it is called a recurrent tumor. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence).
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it. After this testing is done, you and your child’s doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, radiation therapy, or chemotherapy, but they may be used in a different combination or given at a different pace. Your child’s doctor may suggest clinical trials that are studying new ways to treat recurrent medulloblastoma. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
Treatment of recurrent medulloblastoma depends on 2 factors:
-
Whether the tumor recurred in the place where it began or in another part of the brain
-
The type of treatment the child received for the original tumor
Depending on each child’s situation, the doctor may recommend surgery, radiation therapy, chemotherapy, and/or other therapies. Salvage chemotherapy refers to the use of chemotherapy for a patient who experiences a recurrence following initial treatment in the hope of providing a cure or prolonging the person's life.
If your child is diagnosed with a recurrence, you and your family may experience emotions such as disbelief or fear. You are encouraged to talk with your child’s health care team about these feelings and ask about support services to help your family cope. Learn more about dealing with a recurrence .
Return to top
If treatment does not work
Although treatment is successful for many children with a brain tumor, sometimes it is not. If medulloblastoma cannot be cured or controlled, this is called advanced or terminal medulloblastoma. This diagnosis is stressful, and advanced medulloblastoma may be difficult to discuss. However, it is important to have open and honest conversations with your child’s health care team to express your family’s feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help.
Hospice care is designed to provide the best possible quality of life for people who are expected to live less than 6 months. Parents and guardians are encouraged to talk with the health care team about hospice options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Some children may be happier and more comfortable if they can attend school part-time or keep up other activities and social connections. The child’s health care team can help parents or guardians decide on an appropriate level of activity. Making sure a child is physically comfortable and free from pain is extremely important as part of end-of-life care. Learn more about caring for a terminally ill child and advanced care planning .
The death of a child is an enormous tragedy, and families may need support to help them cope with the loss. Pediatric cancer centers often have professional staff and support groups to help with the process of grieving. Learn more on grieving the loss of a child .
Return to top
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for children with medulloblastoma. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - About Clinical Trials
ON THIS PAGE: You will learn more about clinical trials, which are the main way that new medical approaches are studied to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to care for children with medulloblastoma. To make scientific advances, doctors create research studies involving volunteers, called clinical trials. Every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials.
Clinical trials are used for all types and stages of medulloblastoma. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of existing treatments, new approaches to radiation therapy or surgery, and new methods of treatment.
Children who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and the chance that the new treatment may not work. People are encouraged to talk with their health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment. Talk with your child's doctor about clinical trials for symptoms and side effects.
Deciding to join a clinical trial
People decide to participate in clinical trials for many reasons. For some, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the added uncertainty of a clinical trial in the hope of a better result. Others volunteer for clinical trials because they know that these studies are a way to contribute to the progress in treating medulloblastoma. Even if they do not benefit directly from the clinical trial, their participation may benefit future people with medulloblastoma.
Insurance coverage and the costs of clinical trials differ by location and by study. In some programs, some of the expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team and your insurance company first to learn if and how your child’s treatment in a clinical trial will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, their child may receive no treatment by being given a placebo or a “sugar pill.” You and your child will always be told when a placebo is used in a study. Find out more about placebos in cancer clinical trials .
Patient safety and informed consent
To join a clinical trial, parents and children must participate in a process known as informed consent. Informed consent means that parents give permission for their child to participate in a clinical trial and that teenagers give their consent to participate. During informed consent, the doctor should:
-
Describe all of the treatment options so that the person understands how the new treatment differs from the standard treatment.
-
List all of the risks of the new treatment, which may or may not be different than the risks of standard treatment.
-
Explain what will be required of each person in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
-
Describe the purposes of the clinical trial and what researchers are trying to learn.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together. Your child will need to meet all of the eligibility criteria in order to participate in a clinical trial. Learn more about eligibility criteria in clinical trials.
People who participate in a clinical trial may stop participating at any time for personal or medical reasons. This may include that the new treatment is not working or there are serious side effects. Clinical trials are also closely monitored by experts who watch for any problems with each study. It is important that people participating in a clinical trial talk with the doctor and researchers about who will be providing treatment and care during the clinical trial, after the clinical trial ends, and/or if they choose to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of tumors. For specific topics being studied for medulloblastoma, learn more in the Latest Research section.
Cancer.Net offers more information about clinical trials in other areas of the website, including a complete section on clinical trials and places to search for clinical trials for a specific type of tumor .
In addition, you can find a free video-based educational program about clinical trials in another section of this website.
The next section in this guide is Latest Research . It explains areas of scientific research for medulloblastoma. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Latest Research
ON THIS PAGE: You will read about the scientific research being done to learn more about medulloblastoma and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about medulloblastoma, ways to prevent it, how to best treat it, and how to provide the best care to children diagnosed with this disease. The following areas of research may include new options for patients through clinical trials. Always talk with your child’s doctor about the best diagnostic and treatment options for your child.
-
New staging systems. In addition to the staging criteria currently used (see Stages ), newer factors are being examined to help stage medulloblastoma in order to choose treatment. For example, tumors with certain features are being treated as high-risk tumors in some clinical trials. This includes features that are called anaplastic and changes to certain genes, such as MYC and MYCN.
-
Biomarker testing of the tumor. Researchers are looking at laboratory tests for tumor samples to identify specific genes, proteins, and other factors unique to medulloblastoma. It is now known that medulloblastoma is made up of 4 subtypes:
-
WNT
-
SHH
-
Group 3
-
Group 4
Results from these studies may help develop specific treatments for each type of medulloblastoma. This could include new drugs that target factors that help medulloblastoma grow and spread. Such drugs are being tested for patients with a tumor that comes back after initial treatment. These molecular features are also being looked at to predict how well treatment will work. Future studies will likely base treatment on each tumor’s specific molecular features. Learn more about this approach, called targeted therapy .
-
-
Improved methods of imaging and surgery. Imaging techniques have been developed that help surgeons pinpoint the tumor’s location. Using these techniques may reduce or prevent damage to the healthy parts of the brain during treatment.
Functional MRI (fMRI) is an imaging technique that identifies the parts of the brain that control speech, hearing, vision, touch, and movement. The specific locations of these functions are slightly different in each person, so fMRI allows surgeons to plan surgery around these areas.
Image-guided stereotaxis allows surgeons to visualize and operate on the brain using 3-dimensional outlines of the brain and the tumor. Along with specialized software, these images help guide the surgeon to the tumor. Some tumors that were once considered inoperable can now be removed by using this technique.
-
Improved methods of delivering radiation treatment. Conformal radiation therapy is a way to deliver high doses of radiation therapy more directly to a tumor and avoid healthy tissue. This technique produces detailed, 3-dimensional maps of the brain and tumor so doctors know exactly where to deliver the radiation therapy.
-
Combination of therapies. Other areas of research include studies that examine the safety of reducing the doses of radiation therapy for children with a standard-risk tumor by using new approaches to chemotherapy. Other studies in infants and older children with a high-risk tumor focus on new drugs and combinations of radiation therapy and chemotherapy to slow or stop tumor growth.
-
Palliative care/supportive care. Clinical trials are underway to find better ways of reducing symptoms and side effects of current medulloblastoma treatments to improve comfort and quality of life for patients.
Looking for More About the Latest Research?
If you would like more information about the latest areas of research in childhood brain tumors, explore these related items that take you outside of this guide.
-
To find clinical trials specific to your child’s diagnosis, talk with your child’s doctor or search online clinical trial databases .
-
Visit the website of Conquer Cancer, the ASCO Foundation , to find out how to help support cancer research. Please note that this link takes you to a different ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance on how to cope with the physical, emotional, social, and financial changes that medulloblastoma and its treatment can bring. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Coping with Treatment
ON THIS PAGE: You will learn more about coping with the physical, emotional, social, and financial effects of a childhood brain tumor and its treatment. Use the menu to see other pages.
Every treatment for a brain tumor can cause side effects or changes to your child’s body and how they feel. For many reasons, people do not experience the same side effects even when they are given the same treatment for the same tumor type. This can make it hard to predict how your child will feel during treatment.
As your family prepares to start treatment, it is normal to fear treatment-related side effects . It may help to know that your health care team will work to prevent and relieve side effects. This part of treatment is called palliative care or supportive care. It is an important part of your child’s treatment plan, regardless of their age or the stage of disease.
Coping with physical side effects
Common physical side effects from each treatment option for medulloblastoma are listed in the Types of Treatment section. Learn more about side effects of a brain tumor and its treatment, along with ways to prevent or control them . Changes to your child’s physical health depend on several factors, including the tumor’s stage, the length and dose of treatment, and your child’s general health.
It is important to discuss any new side effects or changes in existing side effects with your child’s health care team. Providing this information helps them find ways to treat or manage the side effects so your child feels more comfortable and can potentially keep any side effects from worsening.
You may find it helpful to keep track of your child’s side effects so you are prepared to discuss any changes with the health care team. Learn more about why tracking side effects is helpful .
Sometimes, side effects can last after treatment ends. Doctors call these long-term side effects. Side effects that occur months or years after treatment are called late effects . Treating long-term side effects and late effects is an important part of care for childhood cancer survivors. Learn more by reading the Follow-Up Care section of this guide or talking with your child’s doctor.
Coping with emotional and social effects
Your family can have emotional and social effects after a diagnosis of medulloblastoma. This may include dealing with a variety of emotions, such as anxiety, sadness, or anger, or managing your stress. Sometimes, people find it difficult to express how they feel to their loved ones. Some have found that talking to an oncology social worker, counselor, or member of the clergy can help them develop more effective ways of coping and talking about the diagnosis.
You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your family’s needs.
Coping with the costs of medical care
Treatment for medulloblastoma can be expensive. It can be a source of stress and anxiety for families dealing with a diagnosis. In addition to treatment costs, many people find they have extra, unplanned expenses related to their child’s care. Families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations in a separate part of this website.
Coping with barriers to care
Some groups of people experience different rates of new cancer cases and experience different outcomes from their cancer diagnosis. These differences are called “cancer disparities.” Disparities are caused in part by real-world barriers to quality medical care and social determinants of health , such as where a person lives and whether they have access to food and health care. Cancer disparities more often negatively affect racial and ethnic minorities , people with fewer financial resources , sexual and gender minorities (LGBTQ+) , adolescent and young adult populations , older adults , and people who live in rural areas or other underserved communities .
If your child is having difficulty getting the care they need, talk with a member of the health care team or explore other resources that help support medically underserved people .
Talking with your child's health care team about side effects
Before starting treatment, talk with your child’s doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they likely to happen?
-
What can we do to prevent or relieve them?
-
When and who should we call about side effects?
Be sure to tell your child's health care team about any side effects that happen during treatment and afterward, too. Tell them even if you do not think the side effects are serious. This discussion should include physical, emotional, social, and financial effects of medulloblastoma.
Caring for a child with medulloblastoma
Family members and friends often play an important role in taking care of a child with medulloblastoma. This is called being a caregiver. As a parent or guardian, you are the primary caregiver for your child. However, friends and family members can give your family valuable support, even if they live far away.
When your child has medulloblastoma, you may have an additional range of responsibilities. These may include giving medications or managing symptoms and side effects. However, it is important to seek help from others. Below are some of the responsibilities your family or friends could help with:
-
Providing short-term care for your child
-
Giving support and encouragement
-
Assisting with meals or household chores
-
Helping with insurance and billing issues
A caregiving plan can help caregivers stay organized and help identify opportunities to delegate tasks to others. Ask how much care your child may need at home and with daily tasks during and after treatment. Use this 1-page fact sheet that includes an action plan to help make caregiving a team effort. This free fact sheet is available as a PDF, so it is easy to print.
Learn more about caregiving or read the ASCO Answers Guide to Caring for a Loved One With Cancer in English or Spanish .
Looking for More on How to Track Side Effects?
Cancer.Net offers several resources to help you keep track of symptoms and side effects. Please note that these links will take you to other sections of Cancer.Net:
-
Cancer.Net Mobile: The free Cancer.Net mobile app allows you to securely record the time and severity of your child's symptoms and side effects.
-
ASCO Answers Managing Pain: Get this 32-page booklet about the importance of pain relief that includes a pain tracking sheet to record how pain affects your child. The free booklet is available as a PDF, so it is easy to print.
-
ASCO Answers Fact Sheets: Read 1-page fact sheets on anxiety and depression , constipation , diarrhea , and rash that provide a tracking sheet to record details about the side effect. These free fact sheets are available as a PDF, so they are easy to print, fill out, and give to your health care team.
The next section in this guide is Follow-Up Care . It explains the importance of checkups after your child finishes treatment for medulloblastoma. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Follow-Up Care
ON THIS PAGE: You will read about your child’s medical care after treatment is finished and why this follow-up care is important. Use the menu to see other pages.
Care for children diagnosed with medulloblastoma does not end when active treatment has finished. Your child’s health care team will continue to check that the tumor has not come back, manage any side effects, and monitor your child’s overall health. This is called follow-up care. All children treated for medulloblastoma should have life-long, follow-up care.
Your child’s follow-up care may include regular physical examinations, medical tests, or both. Doctors want to keep track of your child’s recovery in the months and years ahead.
Cancer rehabilitation may be recommended, and this could mean any of a wide range of services such as physical therapy, family or individual counseling, nutritional planning, and/or educational assistance. The goal of rehabilitation is to help survivors and their families regain control over many aspects of their lives and remain as independent as possible. Learn more about cancer rehabilitation.
Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence, which means that the tumor has come back. A tumor recurs because small areas of cancer cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms.
During follow-up care, a doctor familiar with your child’s medical history can give you personalized information about the risk of recurrence. The doctor will ask specific questions about your child’s health. Some children may have blood tests or imaging tests as part of regular follow-up care, but testing recommendations depend on several factors, including the type of tumor and stage first diagnosed and the types of treatment given.
The anticipation before having a follow-up test or waiting for test results may add stress to you or a family member. This is sometimes called “scanxiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects of medulloblastoma
Sometimes, side effects may linger beyond the active treatment period. These are called long-term side effects. In addition, other side effects called late effects may develop months or even years after treatment has ended. Late effects can occur almost anywhere in the body. They include physical problems, such as heart and lung problems, and second cancers, which is a new cancer that happens in someone who has had cancer before. They also include emotional problems, such as anxiety, depression, and problems with memory, thinking, attention, and learning difficulties.
Based on the type of treatment your child received, the doctor will recommend what examinations and tests are needed to check for late effects and side effects from surgery. Late effects of treatment for medulloblastoma can include cognitive and hormonal symptoms from radiation therapy to the brain or spinal cord. Follow-up care should address your child’s quality of life, including any developmental or emotional concerns.
The Children's Oncology Group (COG) has studied the physical and psychological effects that childhood cancer survivors face. Based on these studies, COG has created recommendations for long-term follow-up care for childhood, adolescent, and young adult cancer survivors that can be found on a separate website: www.survivorshipguidelines.org .
Keeping a child’s personal health record
You are encouraged to organize and keep a personal record of your child’s medical information. The doctor will help you create this. That way, as the child enters adulthood, they have a clear, written history of the diagnosis, the treatments, and the doctor’s recommendations about the schedule for follow-up care. The American Society of Clinical Oncology (ASCO) offers forms to help create a treatment summary to keep track of the treatment your child received and develop a survivorship care plan when treatment is completed.
Some children continue to see their oncologist, while others transition back to the care of their pediatrician, primary care doctor, or another health care professional. This decision depends on several factors, including the type of tumor and its stage, side effects, health insurance rules, and your family’s personal preferences. Talk with your health care team about your child’s ongoing medical care and any concerns you have about their future health.
If a doctor who was not directly involved in your child’s care for medulloblastoma will lead the follow-up care, be sure to share the treatment summary and survivorship care plan forms with them and with all future health care providers. Details about the specific treatment given are very valuable to the health care professionals who will care for your child throughout their lifetime.
The next section in this guide is Survivorship . It describes how to cope with challenges in everyday life after a diagnosis of medulloblastoma. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Survivorship
ON THIS PAGE: You will read about how to cope with challenges in everyday life after your child’s medulloblastoma diagnosis. Use the menu to see other pages.
What is survivorship?
The word “survivorship” means different things to different people, but it often describes living with, through, and beyond cancer. In some ways, survivorship is one of the most complicated parts of the cancer experience because it is different for every child and their family.
After active treatment ends, children and their families may experience a mixture of strong feelings, including joy, concern, relief, guilt, and fear. Some people say they appreciate life more after a diagnosis of medulloblastoma. Other families stay very anxious about their child’s health and become uncertain about coping with everyday life.
One source of stress may occur when frequent visits to the health care team end after completing treatment. Often, relationships built with the health care team provide a sense of security during treatment, and children and their families miss this source of support. This may be especially true when new worries and challenges surface over time, such as any late effects of treatment, learning or school problems, emotional challenges, sexual health and fertility concerns, and/or financial issues.
Every family faces different concerns and challenges. With any challenge, a good first step is being able to recognize each fear and talk about it. Effective coping requires:
-
Understanding the challenge your family is facing
-
Thinking through solutions
-
Asking for and allowing the support of others
-
Feeling comfortable with the course of action your family chooses
It may be helpful to join an in-person support group or online community of childhood central nervous system (CNS) tumor survivors. Support groups also exist for parents of children diagnosed with a CNS tumor. This allows you to talk with people who have had similar first-hand experiences. Other options for finding support include talking with a friend or member of your health care team, individual counseling, or asking for assistance at the learning resource center of the place where your child received treatment.
Healthy living after medulloblastoma
Survivorship often serves as a strong motivator to make lifestyle changes, often for the whole family.
Children who have had medulloblastoma can enhance the quality of their future by following established guidelines for good health into and through adulthood, including not smoking, limiting alcohol, maintaining a healthy weight, eating well, managing stress, and participating in regular physical activity. Talk with the doctor about developing a plan that is best for your child’s needs. Learn more about making healthy lifestyle choices .
It is important that your child has recommended medical checkups and tests (see Follow-Up Care ) to take care of their health.
Talk with your health care team to develop a survivorship care plan that is best for your child’s needs.
Changing role of caregivers
Parents, other family members, and friends may also go through periods of transition. A caregiver plays a very important role in supporting a child diagnosed with medulloblastoma, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver's role often changes. Eventually, the need for caregiving related to a child’s diagnosis will become much less or come to an end as your child gets older. Family counselors at pediatric cancer centers can help with this transition. You can also learn more about adjusting to life after caregiving .
Looking for More Survivorship Resources?
For more information about survivorship, explore these related items. Please note these links will take you to other sections of Cancer.Net:
-
Survivorship Resources: Cancer.Net offers information and resources to help survivors cope, including specific sections for children and teens and young adults . There is also a main section on survivorship for people of all ages.
-
ASCO Answers Guide to Cancer Survivorship: Get this 48-page booklet that can help with the transition into life after treatment. It includes blank treatment summary and survivorship care plan forms. The free booklet is available as a PDF, so it is easy to print.
The next section offers Questions to Ask the Health Care Team to help start conversations with your child’s medical team. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Questions to Ask the Health Care Team
ON THIS PAGE: You will find some questions to ask your child’s doctor or other members of the health care team, to help you better understand your child’s diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with the health care team is important to make informed decisions about your child’s care. These suggested questions are a starting point to help you learn more about your child’s care and treatment. You are also encouraged to ask additional questions that are important to you. You may want to print this list and bring it to your child’s next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your child’s care. It may also be helpful to ask a family member or friend to come with you to appointments to help take notes.
Questions to ask after getting a diagnosis
-
What type of tumor has been diagnosed?
-
Is the tumor cancerous?
-
What is the exact location?
-
What is the stage or risk group of the tumor? What does this mean?
-
What is the molecular subtype of my child’s tumor?
-
Can you explain my child’s pathology report (laboratory test results) to me?
Questions to ask about choosing a treatment and managing side effects
-
What is your familiarity with my child’s tumor type and its treatment?
-
What treatment options are available to my child?
-
What clinical trials are available for my child? Where are they located, and how do I find out more about them?
-
What treatment plan do you recommend? Why?
-
What is the goal of each treatment? Is it to eliminate the tumor, help my child feel better, or both?
-
Who will be part of my child’s health care team, and what does each member do?
-
Who will be leading my child’s overall treatment?
-
What are the possible side effects of each treatment, both in the short term and the long term?
-
How will this treatment affect my child’s daily life? Will they be able to go to school and perform their usual activities?
-
Could this treatment affect my child’s ability to become pregnant or have children in the future? If so, should I talk with a fertility specialist before treatment begins?
-
If I’m worried about managing the costs of medical care, who can help me?
-
What follow-up tests will my child need, and how often will those tests be needed?
-
What support services are available to me? To my family?
-
If I have questions or problems, who should I call?
Questions to ask about having surgery
-
What type of surgery will my child have?
-
How long will the operation take?
-
How long will my child be in the hospital?
-
Can you describe what my child’s recovery from surgery will be like?
-
What are the possible long-term effects of having this surgery?
Questions to ask about having radiation therapy
-
What type of treatment is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
What side effects can my child expect during or after each treatment?
-
Who should I contact about any side effects my child experiences? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about having chemotherapy or other medications
-
What type of treatment is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
Will my child receive this treatment at a hospital or clinic? Or will they take it at home?
-
What side effects can my child expect during or after each treatment?
-
Who should I contact about any side effects my child experiences? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about planning follow-up care
-
What is the chance that the tumor will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the treatment my child received?
-
What follow-up tests will my child need, and how often will those tests be needed?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
Who will be leading my child’s follow-up care?
-
What survivorship support services are available to my child? To my family?
The next section in this guide is Additional Resources . It offers more resources on this website that may be helpful to you. Use the menu to choose a different section to read in this guide.
Medulloblastoma - Childhood - Additional Resources
ON THIS PAGE: You will find some helpful links to other areas of Cancer.Net that provide information about medical care and treatment. This is the final page of Cancer.Net’s Guide to Childhood Medulloblastoma. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of medulloblastoma for the person diagnosed and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Here are a few links to help you explore other parts of Cancer.Net:
-
Search for a specialist in your local area using this free database of doctors from the American Society of Clinical Oncology (ASCO).
-
Learn what phrases and terms used in medical care and treatment mean.
-
Read more about the first steps to take when your child is diagnosed with a tumor .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of medical care.
-
Learn more about coping with the emotions that a tumor can bring, including those within a family or a relationship.
-
Find national, not-for-profit advocacy organizations that may offer additional information, services, and support about medulloblastoma and childhood cancers .
-
Explore what to do when your child finishes active treatment .
-
Download Cancer.Net Mobile , a free app that includes a symptom and side effect tracker, medication reminders, and other interactive resources.
-
To find a range of information and insights from different voices on timely topics, visit the Cancer.Net Blog .
-
Watch Cancer.Net videos with ASCO experts explaining the basics of cancer treatment, side effects, survivorship, clinical trials, caregiving, and more.
This is the end of Cancer.Net’s Guide to Childhood Medulloblastoma. Use the menu to choose a different section to read in this guide.













