Leukemia - Acute Lymphocytic - ALL - Introduction
Editorial Note: Please note that this section is currently under review and will be updated soon.
ON THIS PAGE : You will find some basic information about this disease and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Adult Acute Lymphocytic Leukemia. Use the menu to see other pages. Think of that menu as a roadmap for this complete guide.
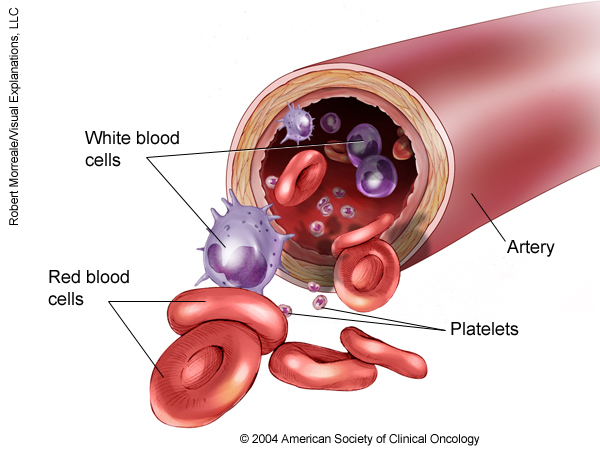
Leukemia is a cancer of the blood. Leukemia begins when healthy blood cells change and grow out of control. Acute lymphocytic leukemia (ALL) is a cancer of the immature lymphocytes. Lymphocytes are a type of white blood cell involved in the body’s immune system. ALL is also called acute lymphoid leukemia or acute lymphoblastic leukemia. Acute means that the disease begins and gets worse quickly. People with ALL usually need immediate treatment. ALL is most common in young children and adults older than 50, but people of any age can develop ALL.
About lymphocytes
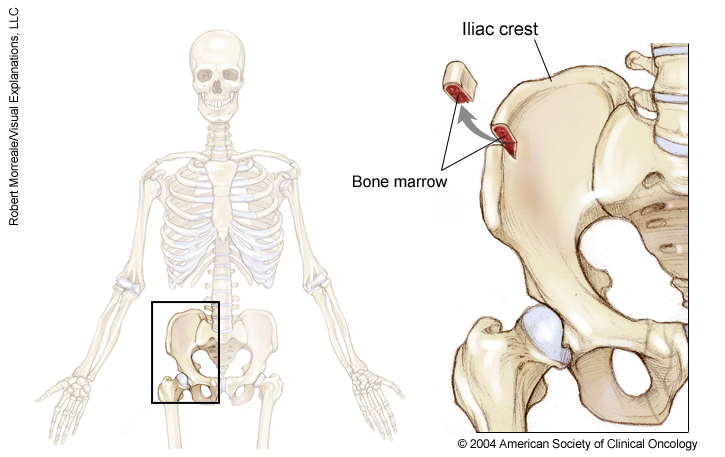
Lymphocytes are made in the bone marrow, the spongy, red tissue in the inner part of the large bones. Lymphocytes are found in the blood, lymph nodes, and spleen. Healthy lymphocytes fight bacterial and viral infections. In people with ALL, new lymphocytes do not develop into mature cells, but stay as immature cells called lymphoblasts.
There are 3 different types of lymphocytes: B cells, T cells, and natural killer (NK) cells.
-
B cells make antibodies.
-
T cells fight infections by activating other cells in the immune system and by destroying infected cells.
-
NK cells fight microbes and cancer cells.
About 85% of people with ALL have the B-cell subtype and about 15% have the T-cell type. The NK-cell subtype is quite rare.
About ALL
In people with ALL, the abnormal cells crowd other types of cells in the bone marrow. This prevents the production of the following cells:
-
Red blood cells, which carry oxygen
-
Other types of white blood cells
-
Platelets, which are parts of the blood needed for clotting
This means that people with ALL may have problems related to having too few healthy blood cells, including:
-
Anemia, from not enough red blood cells
-
Infections because they do not have enough of the type of white blood cells called neutrophils that fight bacteria
-
Increased risk of bruises or bleeding because of a low level of platelets
Lymphoblasts may also collect in a person’s lymphatic system and cause swelling of the lymph nodes. Some cells may invade other organs, including the brain, liver, spleen, thymus, or the testicles in men.
Unlike other types of cancer, the spread of ALL to other parts of the body does not mean the cancer is in an advanced stage. Acute leukemia is usually found throughout the body when it is diagnosed and it may still be cured.
This section is about ALL in adults. Read about childhood ALL .
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
Cancer.Net Patient Education Video: View a short video led by an ASCO expert in leukemia that provides basic information and areas of research.
-
Cancer.Net En Español: Read about ALL in Spanish . Infórmase sobre leucemia linfocítica aguda en español .
The next section in this guide is Statistics . It helps explain the number of people who are diagnosed with this disease and general survival rates. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Statistics
ON THIS PAGE: You will find information about the estimated number of people who will be diagnosed with acute lymphocytic leukemia (ALL) each year. You will also read general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with cancer are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this cancer and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for you individually. The original sources for these statistics are provided at the bottom of this page.
How many people are diagnosed with ALL?
While leukemia in general is a common disease, the specific subtype of ALL is uncommon, making up less than half of 1% of cancers diagnosed in the United States. In 2023, an estimated 6,540 people of all ages (3,660 men and boys and 2,880 women and girls) in the United States will be diagnosed with ALL.
A person of any age can be diagnosed with ALL, but most cases occur in children. In children and teens under age 20, ALL is the most common type of leukemia, accounting for 75% of all leukemia diagnosed in this age group. Children younger than 5 have the highest risk of ALL. (Learn more about childhood ALL statistics .) After a child grows into adulthood, the general risk of ALL rises again after age 50. About 4 out of every 10 people diagnosed with ALL are adults.
It is estimated that 1,390 deaths (700 men and boys and 690 women and girls) from this disease will occur in the United States in 2023. The majority (about 80%) will be in adults.
What is the survival rate for ALL?
There are different types of statistics that can help doctors evaluate a person’s chance of recovery from ALL. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having cancer may affect life expectancy. Relative survival rate looks at how likely people with ALL are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this cancer.
Example: Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) will be alive in 5 years.
It is important to remember that statistics on the survival rates for people with ALL are only an estimate. They cannot tell an individual person if cancer will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
The 5-year relative survival rate for people age 20 and older is 43%. The 5-year relative survival rate for people under age 20 is 90%.
Recent advances in treatment have significantly lengthened the lives of people with ALL. However, the survival rates for the disease vary based on several factors. These include the
biological features
of subtype and classification of the cancer, a person’s age and general health, and how well the treatment plan works.
Experts measure relative survival rate statistics for ALL every 5 years. This means the estimate may not reflect the results of advancements in how ALL is diagnosed or treated from the last 5 years. Talk with your doctor if you have any questions about this information. Learn more about
understanding statistics
.
Statistics adapted from the American Cancer Society’s (ACS) publication Cancer Facts & Figures 2023, and the ACS website. (All sources accessed February 2023.)
The next section in this guide is Medical Illustrations . It offers drawings of body parts often affected by ALL. Use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Medical Illustrations
ON THIS PAGE
: You will find drawings of the main body parts affected by this disease. Use the menu to see other pages.
The next section in this guide is Risk Factors . It explains the factors that may increase the chance of developing ALL. Use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Risk Factors
ON THIS PAGE : You will find out more about the factors that increase the chance of developing ALL. Use the menu to see other pages.
A risk factor is anything that increases a person’s chance of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause cancer. Some people with several risk factors never develop cancer, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor may help you make more informed lifestyle and health care choices.
The cause of ALL is not known. In general, ALL is most likely to affect children and older adults. The following factors may raise a person’s risk of developing ALL:
-
Age. Children younger than 15 and adults older than 50 are more likely to develop ALL.
-
Race. White people are somewhat more likely than black people to develop ALL for reasons that are not understood.
-
Genetic conditions. People with some genetic conditions have a higher risk of ALL than the general population. These conditions include the following syndromes:
-
Down syndrome
-
Ataxia telangiectasia
-
Li-Fraumeni syndrome
-
Klinefelter syndrome
-
Fanconi anemia
-
Wiskott-Aldrich syndrome
-
Bloom syndrome
-
High doses of radiation. People who have been exposed to high levels of radiation may be more likely to develop ALL. This includes long-term survivors of atomic bombs. Exposure to electromagnetic fields or high-voltage electric lines has not been proven to increase a person’s risk of ALL. Cell phone use is not a known risk factor for ALL.
-
Viruses. Occasionally, ALL or specific types of lymphoma can be associated with a previous viral infection. Such infections include human T-cell leukemia virus-1 or the Epstein-Barr virus.
According to recent research, many young children who develop ALL may have had genetic changes before birth that are signs of ALL, although it may take several years before the disease develops and causes symptoms. Researchers are studying this topic to learn more.
The next section in this guide is Symptoms and Signs . It explains what body changes or medical problems this disease can cause. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Symptoms and Signs
ON THIS PAGE : You will find out more about body changes and other things that can signal a problem that may need medical care. Use the menu to see other pages.
People with ALL may experience the following symptoms or signs. Sometimes, people with ALL do not have any of these changes. Or, the cause of a symptom may be a different medical condition that is not cancer.
-
Fatigue
-
Weakness
-
Easy bruising
-
Bleeding that does not stop easily
-
Pale skin
-
Red, pinhead-sized spots on the skin
-
Weight loss
-
Fever
-
Bone, back or abdominal pain
-
Difficulty breathing or shortness of breath
-
Frequent infections or infections that come back
-
Swollen lymph nodes, also called glands
-
Enlarged liver or spleen
-
In women, menstruation that lasts longer than usual
-
Dizziness
-
Headache
-
Blurred vision
-
Nausea and vomiting
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will ask how long and how often you’ve been experiencing the symptom(s), in addition to other questions. This is to help figure out the cause of the problem, called a diagnosis .
If leukemia is diagnosed, relieving symptoms remains an important part of care and treatment. This may also be called symptom management, palliative care, or supportive care. Be sure to talk with your health care team about the symptoms you experience, including any new symptoms or a change in symptoms.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Diagnosis
ON THIS PAGE : You will find a list of common tests, procedures, and scans that doctors use to find the cause of a medical problem. Use the menu to see other pages.
Doctors use many tests to find, or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If this happens, it is called metastasis. For example, imaging tests can show if the cancer has spread. Imaging tests show pictures of the inside of the body. Doctors may also do tests to learn which treatments could work best.
For most types of cancer, a biopsy is the only sure way for the doctor to know whether an area of the body has cancer. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis.
This list describes options for diagnosing this type of cancer. Not all tests listed below will be used for every person. Your doctor may consider these factors when choosing a diagnostic test:
-
The type of cancer suspected
-
Your signs and symptoms
-
Your age and medical condition
-
The results of earlier medical tests
The following tests may be used to diagnose ALL:
-
Blood tests.
If your doctor suspects that you have ALL based on the symptoms, he or she may do a test called a
complete blood count (CBC)
. This test examines the levels of different types of cells in the blood.
Low levels of red blood cells and platelets are common in people with ALL, as are high, normal, or low levels of white blood cells. Changes in blood cell levels can also be a sign of another medical problem that is not leukemia. The blood may also be examined to find out if there are lymphoblasts or other abnormal cells.
-
Bone marrow aspiration and biopsy.
If the blood test shows abnormalities in the number or appearance of the white blood cells, you may need a
bone marrow aspiration and biopsy
. These 2 procedures are similar and often done at the same time to examine the bone marrow. Bone marrow has both a solid and a liquid part. A bone marrow aspiration removes a sample of the fluid with a needle. A bone marrow biopsy is the removal of a small amount of solid tissue using a needle. If blood tests (see above) indicate ALL, it is better to have the bone marrow aspiration and biopsy at the hospital where treatment will be given so the test does not need to be done again.
A pathologist analyzes the sample(s) removed during a bone marrow aspiration and biopsy. A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. The sample is used to look for leukemia, and molecular testing and immunophenotyping (see below) may also be done.
A common site for a bone marrow aspiration and biopsy is the pelvic bone, which is located in the lower back by the hip. The skin in that area is usually numbed with medication beforehand. Other types of anesthesia (medication to block the awareness of pain) may also be used.
-
Other testing.
Your doctor may recommend running laboratory tests on the leukemia cells to identify specific genes, proteins, and other factors unique to the leukemia.
Results of these tests will help decide whether your treatment options include a type of treatment called targeted therapy (see Treatment Options ).
-
Flow cytometry, also called immunophenotyping, and cytochemistry. These tests use chemicals or dyes on the cancer cells to learn more about the leukemia and its subtype. ALL cells have distinctive markers on their surface called cell surface proteins. The pattern of these markers is called the immunophenotype. These tests are used to distinguish ALL from healthy blood cells and from other types of leukemia, which can also involve lymphocytes. Both tests can be done from a blood sample.
-
Karyotyping, or cytogenetics. This test examines a cell’s chromosomes. Chromosomes are long pieces of DNA that contain genes.
People with ALL may have specific chromosomal changes, such as the addition or loss of certain chromosomes and translocations. A translocation is when parts of a chromosome have been moved to another chromosome. These changes can be found with special testing, such as a test called fluorescence in-situ hybridization (FISH). Approximately 25% of patients have a normal karyotype when diagnosed with ALL.
About 20% to 30% of adults with ALL have a specific change in their chromosomes called the Philadelphia chromosome. The Philadelphia chromosome is an example of a small chromosome caused by a translocation. In this instance, it means that genetic material from chromosome 9 breaks off and attaches to chromosome 22 [t(9;22)]. Then, 2 specific genes called BCR and ABL join to make 1 gene called BCR-ABL . Some people may have other types of translocations. For example, many children with ALL have a translocation between chromosomes 12 and 21 [t(12;22)]. These genes are called TEL and AML1 .
-
Molecular assays. These tests may be able to find mutations in genes that cannot be seen with a microscope or found with cytogenetic tests. For example, patients with changes in the IKZF1 gene have a poorer long-term prognosis, which is the chance of recovery. Therefore, testing for these changes during diagnosis helps determine a patient’s treatment options.
-
Lumbar puncture (spinal tap). A lumbar puncture is a procedure in which a doctor uses a needle to take a sample of cerebral spinal fluid (CSF) to look at the make up of the fluid and to find out is it contains cancer cells or blood.
ALL tends to spread to the CSF, which is the fluid that flows around the brain and spinal cord. This means that lumbar punctures are done regularly during ALL treatment. Also, chemotherapy (see Treatment Options ) may be given in the CSF.
Doctors generally give an anesthetic to numb the lower back before the procedure.
-
Imaging tests. The following imaging tests may be used to learn more about the cause of symptoms. They may also help diagnose infections in patients with ALL.
-
Computed tomography (CT or CAT) scan. A CT scan creates a 3-dimensional picture of the inside of the body using x-rays taken from different angles. A computer combines these images into a detailed, cross-sectional view that shows any abnormalities or tumors. Sometimes, a contrast medium (a special dye) is injected into a patient’s vein or given orally (by mouth) to provide better detail.
-
Magnetic resonance imaging (MRI). MRI uses magnetic fields, not x-rays, to produce detailed images of the body. A contrast medium may be injected into a patient’s vein or given orally (by mouth) to create a clearer picture.
-
Positron emission tomography (PET) or PET-CT scan. A PET scan is usually combined with a CT scan (see above), called a PET-CT scan . However, you may hear your doctor refer to this procedure just as a PET scan. A PET scan is a way to create pictures of organs and tissues inside the body. A small amount of a radioactive substance is injected into a patient’s body. This substance is absorbed mainly by organs and tissues that use the most energy. Because cancer tends to use energy actively, it absorbs more of the radioactive substance. A scanner then detects this substance to produce images of the inside of the body.
After diagnostic tests are done, your doctor will review all of the results with you. If the diagnosis is ALL, results can also help the doctor describe the disease. This is called classification .
The next section in this guide is Subtypes and Classification . It explains the system doctors use to describe the extent of the disease. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Subtypes and Classification
ON THIS PAGE : You will learn about how doctors describe ALL. This is called subtype and classification. Use the menu to see other pages.
Doctors divide ALL into subtypes and classify the disease based on the type of lymphocytes that are affected. For example, flow cytometry (see Diagnosis ) distinguishes between ALL involving T cells or B cells. Specific chromosomal or genetic changes in the cancer cells are used to help plan treatment and predict prognosis.
Subtypes include:
-
Precursor B-cell ALL
-
Precursor T-cell ALL
-
Burkitt-type ALL
-
Philadelphia chromosome positive ( BCR-ABL fusion) ALL (see below)
Some patients have a type of leukemia called biphenotypic acute leukemia, also called mixed phenotype acute leukemia or ambiguous lineage acute leukemia. This means that the disease has characteristics of both ALL and/or acute myeloid leukemia (AML) . Often, the same treatments used for ALL are also used for this type of leukemia.
As described in Diagnosis , about 20% to 30% of adults with ALL have a genetic change or mutation called the Philadelphia chromosome (Ph). This causes 2 genes, BCR and ABL, to become 1 fusion gene called BCR-ABL .
The Philadelphia chromosome is found only in the cancerous blood-forming cells, not in other organs of the body. It is not inherited. Therefore, there is no concern about an increased risk of ALL for other family members.
The BCR-ABL gene causes specific types of white blood cells called B lymphoblasts to grow out of control. Knowing whether a person has the BCR-ABL gene helps the doctor predict a patient’s prognosis and recommend treatment. So, it is important to test for it.
About 20% to 25% of patients with precursor B-cell ALL have a type of ALL called Ph-like ALL. The genetic changes found in the leukemia cells of Ph-like ALL act like those linked with the Philadelphia chromosome. But, there are no signs of the Philadelphia chromosome in the leukemia cells. Instead, the leukemia cells have other mutations that act similarly. This means that the same types of treatments used for leukemia with the Philadelphia chromosome may also work for Ph-like ALL.
ALL classification and status of disease
In other types of cancer where a solid tumor forms, doctors agree on a set of stages that describe how big the tumor is and where it has spread. There is no formal staging system for ALL because it usually does not form a solid tumor. And it is often found throughout the body when diagnosed. Instead, there are general classifications used to describe ALL:
-
Newly diagnosed and untreated. The bone marrow contains abnormal lymphoblasts. The person may or may not have any symptoms. A patient often has decreased numbers of healthy white blood cells, red blood cells, and platelets. Some patients may have an overall increased number of white blood cells, but many of these may be abnormal lymphoblasts.
-
In remission. A patient has received treatment for ALL. The bone marrow contains less than 5% blasts, and the patient has no symptoms. The numbers of healthy white blood cells, red blood cells, and platelets are normal. New monitoring methods, called minimal residual disease (MRD; cancer cells not destroyed by treatment) methods, are better able to find small numbers of remaining blasts. MRD methods are now being used more often to determine remission.
-
Refractory. Refractory leukemia means that the disease has not responded to treatment.
-
Recurrent or relapsed ALL. Recurrent leukemia has come back after being in remission. If the leukemia does return, there will be another round of tests to learn about the extent of the recurrence. These tests and scans are often similar to those done at the time of the original diagnosis .
The subtype and classification of ALL will help the doctor recommend a specific treatment plan. The next section in this guide is Treatment Options . You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Treatment Options
ON THIS PAGE : You will learn about the different treatments doctors use for people with ALL. Use the menu to see other pages.
This section tells you the treatments that are the standard of care for this type of leukemia. “Standard of care” means the best treatments known. When making treatment plan decisions, patients are encouraged to consider clinical trials as an option. A clinical trial is a research study that tests a new approach to treatment. Doctors want to learn whether the new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Your doctor can help you consider all your treatment options. To learn more about clinical trials, see the About Clinical Trials and Latest Research sections.
Treatment overview
In cancer care, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team . Cancer care teams include a variety of other health care professionals, such as physician assistants, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Descriptions of the most common treatment options for ALL are listed below. Treatment options and recommendations depend on several factors, including the subtype and classification of ALL, possible side effects, the patient’s preferences and overall health. Your care plan may also include treatment for symptoms and side effects, an important part of cancer care. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. Learn more about making treatment decisions .
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by ending the cancer cells’ ability to grow and divide.
Chemotherapy is given by a medical oncologist or a hematologist. A medical oncologist is a doctor who specializes in treating cancer with medication. A hematologist is a doctor who specializes in treating blood disorders.
Systemic chemotherapy gets into the bloodstream to reach cancer cells throughout the body. Common ways to give chemotherapy include:
-
An intravenous (IV) tube placed into a vein using a needle. It may be given into a larger vein or a smaller vein, such as in the arm. When it is given into a larger vein, a central venous catheter or port may need to be placed in the body.
-
An injection given into a muscle
-
In a pill or capsule that is swallowed (orally)
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. Patients with ALL receive several different drugs throughout their treatment.
A patient may receive chemotherapy during different stages of treatment:
- Remission induction therapy. This is the first round of treatment given during the first 3 to 4 weeks after diagnosis. It is designed to destroy most of the leukemia cells, stop symptoms of the disease, and return the blood counts to normal levels.
The specific treatments used may include:
-
Daunorubicin (Cerubidine)
-
Doxorubicin (Adriamycin), cyclophosphamide (Neosar), or vincristine (Vincasar), given by an injection into a vein
-
Asparaginase (Elspar) or Pegasparaginase (Oncaspar), given by injection into a muscle, under the skin or into a vein
-
Dexamethasone (multiple brand names) or prednisone (multiple brand names) by mouth
-
Methotrexate (multiple brand names) or cytarabine (Cytosar-U) as an injection into the spinal fluid
-
Treatments that targeted the Philadelphia chromosome (see Targeted therapy, below)
The goal of induction therapy is a complete remission (CR). This means that the blood counts have returned to normal, the leukemia cannot be seen when a bone marrow sample is examined under the microscope, and the signs and symptoms of the ALL are gone. More than 95% of children and 75% to 80% of adults with ALL will have a CR.
However, small amounts of leukemia can remain after treatment even if it cannot be seen with a microscope. For this reason, it is necessary to give additional therapy to prevent the ALL from coming back. Techniques can be used to find small amounts of leukemia, called minimal residual disease (MRD). These are used to help predict a patient’s prognosis and guide treatment options.
-
Remission consolidation or intensification therapy. This stage of therapy involves the use of a combination of drugs. The drugs may be different or have different doses than those used to achieve remission. Some drugs may be the same as what was given during remission induction therapy. Depending on the subtype of the ALL, the doctor may recommend several courses of consolidation therapy.
-
Remission maintenance or continuation therapy. Treatment is given both orally and by IV for 2 to 3 years to keep the ALL from returning. These drugs are usually given in lower doses and have fewer side effects.
-
Central nervous system (CNS) prophylaxis (preventive treatment). This is the use of drugs to prevent the leukemia from spreading from the blood to the brain or spinal cord. They are given directly in the spinal fluid by spinal tap (lumbar puncture; see Diagnosis ) and/or by vein. This treatment may be used for a few patients who have leukemia in the CNS when first diagnosed or for some patients with recurrent ALL. This treatment may be given along with radiation therapy to the head and spine.
-
Re-induction chemotherapy. This stage is used to treat ALL if it has come back after treatment. It is also used if a person still has signs of ALL after remission induction therapy.
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells.
Recent studies show that not all cancers have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors involved in your leukemia. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, many research studies are taking place now to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments .
For ALL, targeted therapy is recommended in addition to standard chemotherapy for patients with Philadelphia chromosome-positive ALL (Ph+ ALL). Such drugs include:
-
Imatinib (Gleevec)
-
Dasatinib (Sprycel)
-
Nilotinib (Tasigna)
Other targeted therapy drugs used for ALL include:
-
Ponatinib (Iculsig) for Philadelphia chromosome-positive ALL
-
Nelarabine (Arranon), a new drug that targets T-cell ALL
-
Rituximab (Rituxan), used in addition to chemotherapy for the treatment of B-cell ALL
-
Blinatumumab (Blincyto)
-
Inotuzumab ozogamicin
Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Side effects of chemotherapy and targeted therapy
Induction therapy usually begins in the hospital. Patients will often need to stay in the hospital for 3 to 4 weeks during treatment. However, depending on the situation, many patients can leave the hospital. Those who do, usually need to visit the doctor regularly during treatment.
Some patients will need to stay in the hospital for consolidation therapy but most are able to go home. Many patients with ALL can return to school or work while receiving maintenance therapy.
Chemotherapy attacks rapidly dividing cells, including those in healthy tissue such as the hair, lining of the mouth, intestines, and bone marrow. This means that patients receiving chemotherapy may lose their hair, develop mouth sores, or have nausea and vomiting.
Because of changes in the blood counts, most patients will need transfusions of red blood cells and platelets at some point during their treatment. Treatment with antibiotics to prevent or treat infection is usually needed as well. Chemotherapy may lower the body’s resistance to infection by reducing the number of neutrophils. It can also cause bruising and bleeding because of the decrease in the number of platelets and other problems with blood clotting. Chemotherapy may cause fatigue by lowering the number of red blood cells.
Chemotherapy may affect fertility , which is the ability to have a child in the future, and it increases the risk of developing a second cancer . Patients may want to talk with a fertility specialist before treatment begins, as there are options available to help preserve fertility. Learn more about the basics of chemotherapy and preparing for treatment .
The side effects of targeted therapy include nausea, vomiting, diarrhea, edema or swelling in the legs or around the eyes, and, rarely, fluid in the lungs. The side effects of targeted therapies for ALL are usually not severe and can be managed.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions by using searchable drug databases .
Radiation therapy
Radiation therapy is the use of high-energy x-rays to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. For ALL, radiation therapy to the brain is sometimes used to destroy cancerous cells around the brain and spinal column.
Side effects from radiation therapy may include fatigue, mild skin reactions, upset stomach, and loose bowel movements. Most side effects go away soon after treatment is finished. Learn more about the basics of radiation therapy .
Stem cell transplantation/bone marrow transplantation
A stem cell transplant is a medical procedure in which bone marrow that contains leukemia is destroyed and then replaced by highly specialized cells, called hematopoietic stem cells, that develop into healthy bone marrow. Hematopoietic stem cells are blood-forming cells found both in the bloodstream and in the bone marrow. These stem cells make all of the healthy cells in the blood. Today, this procedure is more commonly called a stem cell transplant, rather than bone marrow transplant, because it is the stem cells in the blood that are typically being transplanted, not the actual bone marrow tissue.
Before recommending transplantation, doctors will talk with the patient about the risks of this treatment and consider several other factors, such as the type of cancer, results of any previous treatment, and patient’s age and general health.
There are 2 types of stem cell transplantation depending on the source of the replacement blood stem cells: allogeneic (ALLO) and autologous (AUTO). ALLO uses donated stem cells, while AUTO uses the patient’s own stem cells. However, AUTO transplants are generally not used to treat ALL. In both types, the goal is to destroy all of the cancer cells in the marrow, blood, and other parts of the body using high doses of chemotherapy and/or radiation therapy and then allow replacement blood stem cells to create healthy bone marrow.
Side effects depend on the type of transplant, your general health, and other factors. Learn more about the basics of stem cell and bone marrow transplantation .
Getting care for symptoms and side effects
ALL and its treatment often cause side effects. In addition to treatments intended to slow, stop, or eliminate the disease, an important part of care is relieving a person’s symptoms and the side effects of treatment. This approach is called palliative or supportive care, and it includes supporting the patient with his or her physical, emotional, and social needs.
Palliative care is any treatment that focuses on reducing symptoms, improving quality of life, and supporting patients and their families. Any person, regardless of age or type and stage of cancer, may receive palliative care. It works best when palliative care is started as early as needed in the cancer treatment process. People often receive treatment for the leukemia at the same time that they receive treatment to ease side effects. In fact, patients who receive both at the same time often have less severe symptoms, better quality of life, and report they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional support, and other therapies. You may also receive palliative treatments similar to those meant to eliminate the leukemia, such as chemotherapy or radiation therapy. Talk with your doctor about the goals of each treatment in the treatment plan.
Before treatment begins, talk with your health care team about the possible side effects of your specific treatment plan and palliative care options. During and after treatment, be sure to tell your doctor or another health care team member if you are experiencing a problem so it can be addressed as quickly as possible. Learn more about palliative care .
Refractory ALL
Refractory ALL occurs when a complete remission is not achieved because the drugs did not destroy enough leukemia cells. These patients often continue to have low blood counts, need transfusions, and have a risk of bleeding or infection.
If you are diagnosed with refractory leukemia, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Also, clinical trials might be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan chosen.
Your treatment plan may include new drugs being tested in clinical trials or ALLO stem cell transplantation. Palliative care will also be important to help relieve symptoms and side effects.
For most patients, a diagnosis of refractory leukemia is very stressful and, at times, difficult to bear. Patients and their families are encouraged to talk about the way they are feeling with doctors, nurses, social workers, or other members of the health care team. It may also be helpful to talk with other patients, including through a support group.
Remission and the chance of recurrence
A remission is when ALL cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it’s important to talk with your doctor about the possibility of the leukemia returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the disease does return. Learn more about coping with the fear of recurrence .
If the leukemia does return after the original treatment, it is called recurrent or relapsed leukemia. When this occurs, a new cycle of testing will begin again to learn as much as possible about the recurrence. After this testing is done, you and your doctor will talk about your treatment options. Often the treatment plan will include the treatments described above, such as chemotherapy, targeted therapy, and radiation therapy, but they may be used in a different combination or given at a different pace. Your doctor may suggest clinical trials that are studying new ways to treat recurrent ALL. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
Treatment for recurrent ALL depends on the length of the remission and is usually given in cycles for 2 to 3 years. If a recurrence occurs after a long remission, the leukemia may respond again to the original treatment. If the remission was short, then other drugs are used. These are often new drugs being tested in clinical trials.
An ALLO stem cell transplant is generally recommended for patients whose leukemia has come back after a second remission. The drug clofarabine (Clolar) may be used for patients between ages 1 and 21 who have recurrent or refractory ALL after already receiving at least 2 types of chemotherapy. Liposomal vincristine (Marqibo) may also be an option. Supportive care will also be important to help relieve symptoms and side effects.
People with recurrent leukemia often experience emotions such as disbelief or fear. Patients are encouraged to talk with their health care team about these feelings and ask about support services to help them cope. Learn more about dealing with cancer recurrence .
If treatment doesn’t work
Recovery from leukemia is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful because the disease is not curable, and for many people, advanced ALL is difficult to discuss. However, it is important to have open and honest conversations with your doctor and health care team to express your feelings, preferences, and concerns. The health care team is there to help, and many team members have special skills, experience, and knowledge to support patients and their families. Making sure a person is physically comfortable and free from pain is extremely important.
Patients who have advanced leukemia and who are expected to live less than 6 months may want to consider a type of palliative care called hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning .
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss .
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for people with cancer. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - About Clinical Trials
ON THIS PAGE : You will learn more about clinical trials, which are the main way that new medical approaches are tested to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to care for patients with ALL. To make scientific advances, doctors create research studies involving volunteers, called clinical trials. In fact, every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials.
Many clinical trials focus on new treatments. Researchers want to learn if a new treatment is safe, effective, and possibly better than the treatment doctors use now. These types of studies evaluate new drugs, different combinations of existing treatments, new approaches to radiation therapy or surgery, and new methods of treatment. Patients who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and that the new treatment may not work. People are encouraged to talk with their health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment. Talk with your doctor about clinical trials for symptoms and side effects. There are also clinical trials studying ways to prevent cancer.
Deciding to join a clinical trial
Patients decide to participate in clinical trials for many reasons. For some patients, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the added uncertainty of a clinical trial in the hope of a better result. Other patients volunteer for clinical trials because they know that these studies are a way to contribute to the progress in treating ALL. Even if they do not benefit directly from the clinical trial, their participation may benefit future patients with ALL.
Insurance coverage of clinical trials costs differs by location and by study. In some programs, some of the patient’s expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team and your insurance company first to learn if and how your treatment in a clinical trial will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, they may receive no treatment by being given a placebo or a “sugar pill.” Placebos are usually combined with standard treatment in most cancer clinical trials. When a placebo is used in a study, it is done with the full knowledge of the participants. Find out more about placebos in cancer clinical trials.
Patient safety and informed consent
To join a clinical trial, patients must participate in a process known as informed consent. During informed consent, the doctor should:
-
Describe all of the patient’s options, so that the person understands how the new treatment differs from the standard treatment.
-
List all of the risks of the new treatment, which may or may not be different from the risks of standard treatment.
-
Explain what will be required of each patient in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together.
Patients who participate in a clinical trial may stop participating at any time for any personal or medical reason. This may include that the new treatment is not working or there are serious side effects. Clinical trials are also closely monitored by experts who watch for any problems with each study. It is important that patients participating in a clinical trial talk with their doctor and researchers about who will be providing their treatment and care during the clinical trial, after the clinical trial ends, and/or if the patient chooses to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of cancer. For specific topics being studied for ALL, learn more in the Latest Research section.
Cancer.Net offers a lot of information about clinical trials in other areas of the website, including a complete section on clinical trials and places to search for clinical trials for a specific type of leukemia .
In addition, this website offers free access to a video-based educational program about clinical trials, located outside of this guide.
The next section in this guide is Latest Research . It explains areas of scientific research currently going on for ALL. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Latest Research
ON THIS PAGE : You will read about the scientific research being done now to learn more about ALL and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about ALL, ways to prevent it, how to best treat it, and how to provide the best care to people diagnosed with this disease. The following areas of research may include new options for patients through clinical trials. Most cancer centers are actively involved in clinical trials aimed at increasing the rate of cure for people with ALL. Always talk with your doctor about the best diagnostic and treatment options for you.
-
New drugs and treatment regimens. Researchers are looking at the use of new types of chemotherapy, as well as different schedules and doses of current drugs. The drug clofarabine has been approved for children with recurrent ALL and is being researched for adults with ALL. The drug bortezomib (Velcade) is also being researched as an option for adults with ALL. In addition, several studies have shown that adolescents and younger to middle-aged adults benefit from the more intensive treatments most often used for younger children with ALL.
-
Immunotherapy and targeted therapy. Immunotherapy , also called biologic therapy, is designed to boost the body’s natural defenses to fight the cancer. It uses materials either made by the body or in a laboratory to improve, target, or restore immune system function. Researchers are studying the use of different antibodies directed against ALL cells, including inotuzumab ozogamicin, blinatumomab, rituximab, and alemtuzumab (Campath). In addition, researchers are looking at a new therapy called chimeric antigen receptor T-cell therapy or CAR T-cell therapy that uses the patient’s T-cells to attack the leukemia cells.
-
Stem cell/bone marrow transplantation. Different ways to make stem cell transplantation (see Treatment Options ) safer and easier are also being studied.
-
Tests to detect small amounts of ALL after treatment. Researchers are studying other molecular or immunologic tests that can help find small amounts of ALL in patients in remission. Then, a change in treatment may prevent the ALL from coming back.
-
Palliative care . Clinical trials are underway to find better ways of reducing symptoms and side effects of current ALL treatments to improve patients’ comfort and quality of life.
Looking for More About the Latest Research?
If you would like additional information about the latest areas of research regarding leukemia, explore these related items that take you outside of this guide:
-
To find clinical trials specific to your diagnosis, talk with your doctor or search online clinical trial databases now .
-
Visit the website of Conquer Cancer, the ASCO Foundation , to find out how to help support cancer research. Please note that this link takes you to a separate ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance in how to cope with the physical, emotional, and social changes that ALL and its treatment can bring. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Coping with Treatment
ON THIS PAGE : You will learn more about coping with the physical, emotional, social, and financial effects of ALL and its treatment. This page includes several links outside of this guide to other sections of this website. Use the menu to see other pages
Every treatment for leukemia can cause side effects or changes to your body and how you feel. For many reasons, people don’t experience the same side effects even when they are given the same treatment for the same type of leukemia. This can make it hard to predict how you will feel during treatment.
As you prepare to start treatment, it is normal to fear treatment-related side effects . It may help to know that your health care team will work to prevent and relieve side effects. Doctors call this part of treatment “palliative care.” It is an important part of your treatment plan, regardless of your age or the subtype and classification of ALL.
Coping with physical side effects
Common physical side effects from each treatment option for ALL are described within the Treatment Options section. Learn more about side effects of leukemia and its treatment, along with ways to prevent or control them . Changes to your physical health depend on several factors, including the leukemia’s subtype and classification, the length and dose of treatment, and your general health.
Sometimes, physical side effects can last after treatment ends. Doctors call these long-term side effects. They call side effects that occur months or years after treatment late effects . Treating long-term side effects and late effects is an important part of survivorship care. Learn more by reading the Follow-up Care section of this guide or talking with your doctor.
Coping with emotional and social effects
You can have emotional and social effects as well as physical effects after a diagnosis of ALL. This may include dealing with difficult emotions, such as sadness, anxiety, or anger, or managing your stress level. Sometimes, patients have problems expressing how they feel to their loved ones, or people don’t know what to say in response.
Patients and their families are encouraged to share their feelings with a member of their health care team. You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your needs.
Coping with financial effects
Cancer treatment can be expensive. It is often a big source of stress and anxiety for people with cancer and their families. In addition to treatment costs, many people find they have extra, unplanned expenses related to their care. For some people, the high cost stops them from following or completing their treatment plan. This can put their health at risk and may lead to higher costs in the future. Patients and their families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations , in a separate part of this website.
Caring for a loved one with ALL
Family members and friends often play an important role in taking care of a person with ALL. This is called being a caregiver. Caregivers can provide physical, practical, and emotional support to the patient, even if they live far away.
Caregivers may have a range of responsibilities on a daily or as-needed basis. Below are some of the responsibilities caregivers take care of:
-
Providing support and encouragement
-
Giving medications
-
Helping manage symptoms and side effects
-
Coordinating medical appointments
-
Providing a ride to appointments
-
Assisting with meals
-
Helping with household chores
-
Handling insurance and billing issues
Learn more about caregiving .
Talking with your health care team about side effects
Before starting treatment, talk with your doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they are likely to happen?
-
What can we do to prevent or relieve them?
Be sure to tell your health care team about any side effects that happen during treatment and afterward, too. Tell them even if you don’t think the side effects are serious. This discussion should include physical, emotional, and social effects of cancer.
Also, ask how much care you may need at home and with daily tasks during and after treatment. This can help you make a caregiving plan.
The next section in this guide is Follow-up Care . It explains the importance of checkups after treatment for ALL is finished. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Follow-Up Care
ON THIS PAGE : You will read about your medical care after treatment for ALL is completed, and why this follow-up care is important. Use the menu to see other pages.
Care for people diagnosed with ALL doesn’t end when active treatment has finished. Your health care team will continue to check to make sure the disease has not returned, manage any side effects, and monitor your overall health. This is called follow-up care.
Your follow-up care may include regular physical examinations, medical tests, or both. Doctors want to keep track of your recovery in the months and years ahead. Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence. ALL recurs because a few leukemia cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms. During follow-up care, a doctor familiar with your medical history can give you personalized information about your risk of recurrence. Your doctor will ask specific questions about your health. Some people may have blood tests or imaging tests done as part of regular follow-up care, but testing recommendations depend on several factors including the subtype of ALL originally diagnosed and the types of treatment given.
The anticipation before having a follow-up test or waiting for test results can add stress to you or a family member. This is sometimes called “scan-xiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects
Most people expect to experience side effects when receiving treatment. However, it is often surprising to survivors that some side effects may linger beyond the treatment period. These are called long-term side effects. Other side effects called late effects may develop months or even years afterwards. Long-term and late effects can include both physical and emotional changes.
Talk with your doctor about your risk of developing such side effects based on the type of leukemia, your individual treatment plan, and your overall health. If you had a treatment known to cause specific late effects, you may have certain physical examinations, scans, or blood tests to help find and manage them.
Keeping personal health records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. ASCO offers forms to help create a treatment summary to keep track of the treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to decide who will lead your follow-up care. Some survivors continue to see their oncologist, while others transition back to the care of their family doctor or another health care professional. This decision depends on several factors, including subtype and classification of ALL, side effects, health insurance rules, and your personal preferences.
If a doctor who was not directly involved in your care for ALL will lead your follow-up care, be sure to share your treatment summary and survivorship care plan forms with him or her, and with all future health care providers. Details about your treatment are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship . It describes how to cope with challenges in everyday life after a diagnosis of ALL. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Survivorship
ON THIS PAGE:
You will read about how to cope with challenges in everyday life after a diagnosis of ALL. Use the menu to see other pages.
What is survivorship?
The word “survivorship” means different things to different people. Common definitions include:
-
Having no signs of cancer after finishing treatment.
-
Living with, through, and beyond cancer. According to this definition, survivorship begins at diagnosis and includes people who continue to have treatment over the long term, to either reduce the risk of recurrence or to manage chronic disease.
Survivorship is one of the most complicated parts of having cancer. This is because it is different for everyone.
Survivors may experience a mixture of strong feelings, including joy, concern, relief, guilt, and fear. Some people say they appreciate life more after the diagnosis and have gained a greater acceptance of themselves. Others become very anxious about their health and uncertain about coping with everyday life.
Survivors may feel some stress when their frequent visits to the health care team end after completing treatment. Often, relationships built with the health care team provide a sense of security during treatment, and people miss this source of support. This may be especially true when new worries and challenges surface over time, such as any late effects of treatment, emotional challenges including fear of recurrence, sexuality and fertility concerns, and financial and workplace issues.
Every survivor has individual concerns and challenges. With any challenge, a good first step is being able to recognize your fears and talk about them. Effective coping requires:
-
Understanding the challenge you are facing
-
Thinking through solutions
-
Asking for and allowing the support of others
-
Feeling comfortable with the course of action you choose
Many survivors find it helpful to join an in-person support group or an online community of survivors. This allows you to talk with people who have had similar first-hand experiences. Other options for finding support include talking with a friend or member of your health care team, individual counseling, or asking for assistance at the learning resource center of the place where you received treatment.
Changing role of caregivers
Family members and friends may also go through periods of transition. A caregiver plays a very important role in supporting a person diagnosed with cancer, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver's role often changes. Eventually, the need for caregiving related to the ALL diagnosis will become much less or come to an end. Caregivers can learn more about adjusting to life after caregiving in this article .
A new perspective on your health
For many people, survivorship serves as a strong motivator to make positive lifestyle changes.
People recovering from ALL are encouraged to follow established guidelines for good health, such as not smoking, limiting alcohol, eating well, and managing stress. Regular physical activity can help rebuild your strength and energy level. Your health care team can help you create an appropriate exercise plan based upon your needs, physical abilities, and fitness level. Learn more about making healthy lifestyle choices .
It is important to have recommended medical checkups and tests (see Follow-up Care ) to take care of your health. Rehabilitation may be recommended, and this could mean any of a wide range of services such as physical therapy, career counseling, pain management, nutritional planning, and/or emotional counseling. The goal of rehabilitation is to help people regain control over many aspects of their lives and remain as independent and productive as possible.
Talk with your doctor to develop a survivorship care plan that is best for your needs.
Looking for More Survivorship Resources?
For more information about survivorship, explore these related items. Please note that these links will take you to other sections of Cancer.Net:
-
ASCO Answers Cancer Survivorship Guide : Get this 44-page booklet that helps people transition into life after treatment. It includes blank treatment summary and survivorship care plan forms. The booklet is available as a PDF, so it is easy to print.
-
Cancer.Net Patient Education Video : View a short video led by an ASCO expert that provides information about what comes next after finishing treatment.
-
Survivorship Resources : Cancer.Net offers an entire area of this website with resources to help survivors, including those in different age groups.
The next section offers Questions to Ask the Health Care Team to help start conversations with your health care team. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Questions to Ask the Health Care Team
ON THIS PAGE : You will find some questions to ask your doctor or other members of your health care team, to help you better understand your diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with your health care team is important to make informed decisions about your health care. These suggested questions are a starting point to help you learn more about your care and treatment. You are also encouraged to ask additional questions that are important to you. You may want to print this list and bring it to your next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your care.
Questions to ask after getting a diagnosis
-
What is my diagnosis? What does this mean?
-
What subtype of ALL do I have?
-
What classification is it?
-
Can you recommend a leukemia specialist?
-
Can you explain my pathology report (laboratory test results) to me?
-
Do I need to start treatment right away?
Questions to ask about choosing a treatment and managing side effects
-
Where is the best place for me to receive treatment?
-
What are my options for treatment?
-
What clinical trials are available for me? Where are they located, and how do I find out more about them?
-
What treatment plan do you recommend? Why?
-
What is the goal of each treatment? Is it to eliminate the leukemia, manage the symptoms and side effects, or both?
-
How long will treatment last?
-
How likely is it that my ALL will go into remission?
-
Who will be part of my health care team, and what does each member do?
-
Who will be leading my overall treatment?
-
What are the possible side effects of this treatment, both in the short term and the long term?
-
Could this treatment affect my sex life? If so, how and for how long?
-
Could this treatment affect my ability to become pregnant or have children? If so, should I talk with a fertility specialist before treatment begins?
-
How will the treatment affect my daily life? Will I be able to work, exercise, and perform my usual activities?
-
If I’m worried about managing the costs of cancer care, who can help me?
-
What support services are available to me? To my family?
-
Whom should I call with questions or problems?
-
Is there anything else I should be asking?
Questions to ask about having chemotherapy, targeted therapy, and radiation therapy
-
What type of treatment is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
Will I need to stay in the hospital at specific times during treatment?
-
What side effects can I expect during treatment?
-
What are the possible long-term effects of having this treatment?
-
What can be done to relieve the side effects?
Questions to ask about planning follow-up care
-
What is the chance that the ALL will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the treatment I received?
-
What follow-up tests will I need, and how often will I need them?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
Who will be leading my follow-up care?
-
What survivorship support services are available to me? To my family?
The next section in this guide is Additional Resources . It offers some more resources on this website beyond this guide that may be helpful to you. You may use the menu to choose a different section to read in this guide.
Leukemia - Acute Lymphocytic - ALL - Additional Resources
ON THIS PAGE : You will find some helpful links to other areas of Cancer.Net that provide information about cancer care and treatment. This is the final page of Cancer.Net’s Guide to Acute Lymphocytic Leukemia in adults. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of leukemia for the person diagnosed and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Beyond this guide, here are a few links to help you explore other parts of Cancer.Net:
-
Search for a specialist in your local area using this free database of doctors from the American Society of Clinical Oncology.
-
Review dictionary articles to help understand phrases and terms used in medical care and treatment .
-
Read more about the first steps to take when you are diagnosed with leukemia .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of medical care.
-
Learn more about coping with the emotions that leukemia can bring, including those within a family or a relationship.
-
Find a national, not-for-profit advocacy organization that may offer additional information, services, and support for people with ALL.
-
Explore what to do when you finish active treatment .
-
To find a range of information and insights from different voices on timely cancer topics, visit the Cancer.Net Blog .
-
For more information about treatment options for this disease, see UpToDate: Patient Information on ALL (Beyond the Basics) . Please note that this link takes you to a separate, independent website.
This is the end of Cancer.Net’s Guide to Adult Acute Lymphocytic Leukemia. You may use the menu to choose a different section to read in this guide.













