Bladder Cancer - Introduction
ON THIS PAGE: You will find some basic information about this disease and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Bladder Cancer. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
About the bladder, renal pelvis, ureter, and urethra (urinary tract)
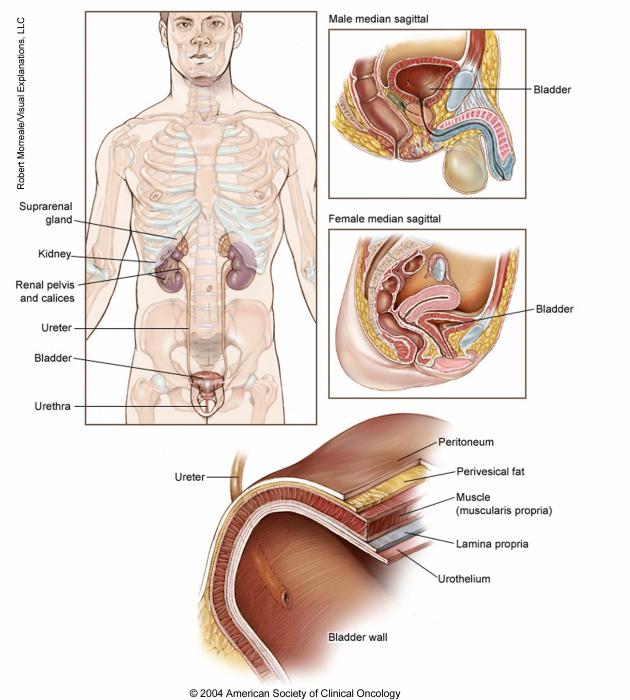
The bladder is a hollow organ in the pelvis that stores urine before it leaves the body during urination. This function makes the bladder an important part of the urinary tract. The urinary tract is also made up of the kidneys, ureters, and urethra. The renal pelvis is a funnel-like part of the kidney that collects urine and sends it into the ureter. The ureter is a tube that runs from each kidney into the bladder. The urethra is the tube that carries urine out of the body. The prostate gland is also part of the urinary tract.
The bladder, like other parts of the urinary tract, is lined with a layer of cells called the urothelium. This layer of cells is separated from the bladder wall muscles, called the muscularis propria, by a thin, fibrous band called the lamina propria.
Bladder cancer begins when healthy cells in the bladder lining—most commonly urothelial cells—change and grow out of control, forming a mass called a tumor. Urothelial cells also line the renal pelvis and ureters and urethra. Cancer that develops in the renal pelvis and ureters is also considered a type of urothelial cancer and is often called upper tract urothelial cancer. In most cases, it is treated in much the same way as bladder cancer and is described in this guide. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but will not spread. Benign bladder tumors are very rare.
Types of bladder cancer
The type of bladder cancer depends on how the tumor’s cells look under the microscope. The 3 main types of bladder cancer are:
-
Urothelial carcinoma. Urothelial carcinoma (or UCC) accounts for about 90% of all bladder cancers. It also accounts for 10% to 15% of kidney cancers diagnosed in adults. It begins in the urothelial cells that line the urinary tract. Urothelial carcinoma used to be called transitional cell carcinoma or TCC.
-
Squamous cell carcinoma. Squamous cells develop in the bladder lining in response to irritation and inflammation. Over time, these cells may become cancerous. Squamous cell carcinoma accounts for about 4% of all bladder cancers.
-
Adenocarcinoma. This type accounts for about 2% of all bladder cancers and develops from glandular cells.
There are other, less common types of bladder cancer, including micropapillary, plasmacytoid, sarcomatoid carcinoma of the bladder , and small cell bladder cancer , among others. Sarcomas of the bladder often begin in the fat or muscle layers of the bladder. Small cell bladder cancer is a rare type of bladder cancer that is likely to spread to other parts of the body.
Other ways of describing bladder cancer
In addition to its cell type, bladder cancer may be described as noninvasive, non-muscle-invasive, or muscle-invasive.
-
Noninvasive. Noninvasive bladder cancer includes noninvasive papillary carcinoma and carcinoma in situ (CIS). Noninvasive papillary carcinoma is a growth found on a small section of tissue that is easily removed. This is called stage Ta. CIS is cancer that is found only on or near the surface of the bladder, which is called stage Tis. See Stages and Grades for more information.
-
Non-muscle-invasive. Non-muscle-invasive bladder cancer typically has only grown into the lamina propria and not into muscle, also called stage I. Non-muscle-invasive cancer may also be called superficial cancer, although this term is being used less often because it may incorrectly suggest that the cancer is not serious.
-
Muscle-invasive. Muscle-invasive bladder cancer has grown into the muscle of the bladder wall and sometimes into the fatty layers or surrounding tissues or organs outside the bladder.
It is important to note that non-muscle-invasive bladder cancer has the potential of spreading into the bladder muscle or to other parts of the body. Additionally, all cell types of bladder cancer can spread beyond the bladder to other areas of the body through a process known as metastasis.
If a bladder tumor has spread into the surrounding organs, such as the uterus, vagina, prostate gland, and/or nearby muscles, it is called locally advanced disease. Bladder cancer also often spreads to the lymph nodes in the pelvis. If it has spread into the liver, bones, lungs, lymph nodes outside the pelvis, or other parts of the body, the cancer is called metastatic disease. This is described in more detail in Stages and Grades .
Looking for More of an Introduction?
If you would like more of an introduction, explore this related item. Please note that this link will take you to another section on Cancer.Net.
-
ASCO Answers Fact Sheet: Read a 1-page fact sheet that offers an introduction to bladder cancer. This free fact sheet is available as a PDF, so it is easy to print.
-
Cancer.Net En Español: Read about bladder cancer in Spanish. Infórmase sobre cáncer de vejiga en español.
The next section in this guide is Statistics . It helps explain the number of people who are diagnosed with bladder cancer and general survival rates. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Statistics
ON THIS PAGE : You will find information about the estimated number of people who will be diagnosed with bladder cancer each year. You will also read general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with cancer are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this cancer and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for you individually. The original sources for these statistics are provided at the bottom of this page.
How many people are diagnosed with bladder cancer?
In 2023, an estimated 82,290 adults (62,420 men and 19,870 women) in the United States will be diagnosed with bladder cancer. Smoking accounts for nearly 50% of all these cases (see Risk Factors ). Worldwide, an estimated 573,278 people were diagnosed with bladder cancer in 2020.
After years of increasing, the number of bladder cancer cases in the United States steadily declined by less than 1% per year from 2004 to 2015 and an estimated 2% per year from 2015 to 2019. Among men, bladder cancer is the fourth most common cancer. Men are 4 times more likely than women to be diagnosed with the disease. In addition, incidence rates in White men are double those of Black, Hispanic, or Asian/Pacific Islander men.
Bladder cancer mostly affects older people. About 90% of people with bladder cancer are older than 55. The average age people are diagnosed with bladder cancer is 73.
It is estimated that 16,710 deaths (12,160 men and 4,550 women) from this disease will occur in the United States in 2023. In 2020, an estimated 212,536 people worldwide died from bladder cancer. Among men in the United States, bladder cancer is the eighth most common cause of cancer death. However, the death rate for bladder cancer decreased by over 2% annually from 2016 to 2020.
What is the survival rate for bladder cancer?
There are different types of statistics that can help doctors evaluate a person’s chance of recovery from bladder cancer. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having cancer may affect life expectancy. Relative survival rate looks at how likely people with bladder cancer are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this cancer.
Example:
Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) will be alive in 5 years.
It is important to remember that statistics on the survival rates for people with bladder cancer are only an estimate. They cannot tell an individual person if cancer will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
The 5-year relative survival rate for bladder cancer in the United States is 77%.
The survival rates for bladder cancer vary based on several factors. These include the stage of cancer, a person’s age and general health, and how well the treatment plan works. Another factor that can affect outcomes is the type of bladder cancer that is diagnosed (see Introduction ).
The 5-year relative survival rate of people with bladder cancer that has not spread beyond the inner layer of the bladder wall is 96%. Almost half of people are diagnosed with this stage.
If the tumor is invasive but has not yet spread outside the bladder, the 5-year relative survival rate is 70%. About 33% of bladders cancers are diagnosed at this stage. If the cancer extends through the bladder to the surrounding tissue or has spread to nearby lymph nodes or organs, the 5-year relative survival rate is 39%. If the cancer has spread to distant parts of the body, the 5-year relative survival rate is 8%. About 5% of people are diagnosed with this stage.
Experts measure relative survival rate statistics for bladder cancer every 5 years. This means the estimate may not reflect the results of advancements in how bladder cancer is diagnosed or treated from the last 5 years. Talk with your doctor if you have any questions about this information. Learn more about understanding statistics .
Statistics adapted from the American Cancer Society's (ACS) publication, Cancer Facts & Figures 2023; the ACS website; and the International Agency for Research on Cancer website. (All sources accessed February 2023.)
The next section in this guide is Medical Illustrations . It offers drawings of the bladder, including its layers of tissue. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Medical Illustrations
ON THIS PAGE: You will find drawings of the bladder and its tissue layers. Use the menu to see other pages.
The next section in this guide is Risk Factors . It describes the factors that may increase the chance of developing bladder cancer. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Risk Factors
ON THIS PAGE: You will find out more about the factors that increase the chance of developing bladder cancer. Use the menu to see other pages.
A risk factor is anything that increases a person’s chance of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause cancer. Some people with several risk factors never develop cancer, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor may help you make more informed lifestyle and health care choices.
The following factors may raise a person’s risk of developing bladder cancer:
-
Tobacco use. The most common risk factor for bladder cancer is cigarette smoking, although smoking cigars and pipes can also raise the risk of developing bladder cancer. Smokers are 4 to 7 times more likely to develop bladder cancer than nonsmokers. Learn more about tobacco’s link to cancer and how to quit smoking .
-
Age. The chances of being diagnosed with bladder cancer increases with age. More than 70% of people with bladder cancer are older than 65.
-
Gender. Men are 4 times more likely to develop bladder cancer than women, but women are more likely to die from bladder cancer than men. Also, women may experience a delayed diagnosis of bladder cancer.
-
Race. White people are more than twice as likely to be diagnosed with bladder cancer as Black people, but Black people are twice as likely to die from the disease.
-
Chemicals. Chemicals used in the textile, rubber, leather, dye, paint, and print industries; some naturally occurring chemicals; and chemicals called aromatic amines and others can also increase the risk of bladder cancer.
-
Previous radiation therapy to the pelvis. People who have been treated for cancer with radiation therapy to the pelvis may have an increased risk of future bladder cancer.
-
Chronic bladder problems. Bladder stones and infections may increase the risk of bladder cancer. Bladder cancer may be more common for people who are paralyzed from the waist down who are required to use urinary catheters and have had many urinary infections.
-
Cyclophosphamide use. People who have had chemotherapy with cyclophosphamide have a higher risk of developing bladder cancer.
-
Pioglitazone (Actos) use. In 2011, the U.S. Food and Drug Administration (FDA) warned that people who have taken the diabetes drug pioglitazone for more than 1 year may have a higher risk of developing bladder cancer. However, published studies have shown contradictory results.
-
Personal history. People who have already had bladder cancer once are more likely to develop bladder cancer again.
-
Schistosomiasis. People who have some forms of this parasitic disease are more likely to develop squamous cell bladder cancer. Schistosomiasis is found in parts of Africa, South America, Southeast Asia, and the Middle East.
-
Lynch syndrome and other genetic syndromes. People with an inherited condition called Lynch syndrome , previously called hereditary nonpolyposis colorectal cancer or HNPCC, or other genetic predisposition may have an increased risk of developing bladder cancer (upper and lower tract). It is important to review your family history of cancer with your doctor.
-
Arsenic exposure. Arsenic is a naturally occurring substance that can cause health problems if consumed in large amounts. When found in drinking water, it has been associated with an increased risk of bladder cancer. The chance of being exposed to arsenic depends on where you live and whether you get your water from a well or from a system that meets the standards for acceptable arsenic levels.
The next section in this guide is Symptoms and Signs . It explains what changes or medical problems bladder cancer can cause. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Symptoms and Signs
ON THIS PAGE: You will find out more about changes and other things that can signal a problem that may need medical care. Use the menu to see other pages.
People with bladder cancer may experience the following symptoms or signs. Symptoms are changes that you can feel in your body. Signs are changes in something measured, like by taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. Sometimes, people with bladder cancer do not have any of the symptoms and signs described below. Or, the cause of a symptom or sign may be a medical condition that is not cancer.
-
Blood or blood clots in the urine
-
Pain or burning sensation during urination
-
Frequent urination
-
Feeling the need to urinate many times throughout the night
-
Feeling the need to urinate, but not being able to pass urine
-
Lower back pain on 1 side of the body
Most often, bladder cancer is diagnosed after a person tells their doctor about blood in the urine, also called hematuria. "Gross hematuria" is a medical term that means that enough blood is present in the urine that the patient can see it. It is also possible that there are small amounts of blood in the urine that cannot be seen. This is called "microscopic hematuria," and it can only be found with a urine test.
General urine tests are not used to make a specific diagnosis of bladder cancer because hematuria can be a sign of several other conditions that are not cancer, such as an infection or kidney stones. One type of urine test that can find out whether there is cancer is cytology, a test in which the urine is studied under a microscope to look for cancer cells (see Diagnosis for more information).
Sometimes when the first symptoms of bladder cancer appear, the cancer has already spread to another part of the body. In this situation, the symptoms depend on where the cancer has spread. For example, cancer that has spread to the lungs may cause a cough or shortness of breath, spread to the liver may cause abdominal pain or jaundice (yellowing of the skin and whites of the eyes), and spread to the bone may cause bone pain or a fracture (broken bone). Other symptoms of advanced bladder cancer may include pain in the back or pelvis, unexplained appetite loss, and weight loss.
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will ask how long and how often you’ve been experiencing the symptom(s), in addition to other questions. This is to help figure out the cause of the problem, called a diagnosis.
If cancer is diagnosed, relieving symptoms remains an important part of cancer care and treatment. Managing symptoms may also be called "palliative care" or "supportive care." It is often started soon after diagnosis and continued throughout treatment. Be sure to talk with your health care team about symptoms you experience, including any new symptoms or a change in symptoms.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Diagnosis
ON THIS PAGE: You will find a list of common tests, procedures, and scans that doctors use to find the cause of a medical problem. Use the menu to see other pages.
Doctors use many tests to find, or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If the cancer has spread, it is called metastasis. Doctors may also do tests to learn which treatments could work best.
For most types of cancer, a biopsy is the only sure way for the doctor to know if an area of the body has cancer. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis.
How bladder cancer is diagnosed
There are many tests used for diagnosing bladder cancer. Not all tests described here will be used for every person. Your doctor may consider these factors when choosing a diagnostic test:
-
The type of cancer suspected
-
Your signs and symptoms
-
Your age and general health
-
The results of earlier medical tests
The earlier bladder cancer is found, the better the chance for successful treatment and cure. However, there is not yet a test accurate enough to screen the general population for bladder cancer, so most people are diagnosed with bladder cancer once they have symptoms . As a result, some people have more advanced (later stage) disease when the cancer is found. Still, most people are usually diagnosed with noninvasive bladder cancer (see Introduction ).
The following tests may be used to diagnose and learn more about bladder cancer:
-
Urine tests. If your doctor has found any amount of blood in the urine, a urine cytology test can be ordered. Urine cytology often uses a random urine sample from normal urination to find out if the urine contains tumor cells. If a patient is undergoing a cystoscopy (see below), an additional test may be performed that involves rinsing the bladder and collecting the liquid through the cystoscope or through another small tube that is inserted into the urethra. The sample can be tested in a variety of ways. The most common way is to look at the cells under a microscope, called urinary cytology. There are other urine tests using molecular analysis that can be done to help find cancer, usually at the same time as urinary cytology.
-
Cystoscopy. Cystoscopy is the key diagnostic procedure for bladder cancer. It allows the doctor to see inside the body with a thin, lighted, flexible tube called a cystoscope. Flexible cystoscopy is performed in a doctor's office and does not require anesthesia, which is medication that blocks the awareness of pain. This short procedure can detect growths in the bladder and determine the need for a biopsy or surgery.
-
Biopsy/Transurethral resection of bladder tumor (TURBT). If abnormal tissue is found during a cystoscopy, the doctor will do a biopsy . A biopsy is the removal of a small amount of tissue for examination under a microscope. This surgical procedure is called a transurethral bladder tumor resection or TURBT.
During a TURBT, the doctor removes the tumor and a sample of the bladder muscle near the tumor. The doctor can also decide to do additional biopsies of other parts of the bladder based on the results of the cystoscopy. Another procedure often done before completing a TURBT is called EUA (exam under anesthesia). In this procedure, the urologist evaluates the bladder to see if any masses can be felt. Any tissue sample removed during the TURBT is then analyzed by a pathologist. A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease.
A TURBT is used to diagnose bladder cancer and find out the type of tumor, how deeply it has grown into the layers of the bladder, and identify any additional microscopic cancerous changes, called carcinoma in situ (CIS) (see Stages and Grades ). A TURBT can also be used as a treatment for a non-muscle-invasive tumor (see Types of Treatment ).
-
Genetic counseling. Some people may have genetic factors that increase their risk for bladder cancer, so speaking with a genetic counselor and developing a detailed family medical history can help identify your potential risk of cancer and that of people in your family, including extended family.
-
Biomarker testing of the tumor. Your doctor may recommend running laboratory tests on a tumor sample to identify specific genes, proteins, and other factors unique to the tumor. This may also be called molecular testing of the tumor. Results of these tests can help determine your treatment options, especially if the cancer has spread.
The following imaging tests may be used to find out if the bladder cancer has spread and to help with staging . Imaging tests show pictures of the inside of the body.
-
Computed tomography (CT or CAT) scan. A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows abnormalities or tumors. A CT scan can be used to measure the tumor’s size and to identify enlarged lymph nodes, which may indicate that cancer has spread. Sometimes, a special dye called a contrast medium is given before the scan to provide better detail on the image. This dye can be injected into a patient’s vein (intravenous) or given as a liquid to swallow. Before taking this test, patients should tell the staff giving this test if they are allergic to iodine or other contrast media. The intravenous contrast dye used in a CT scan can cause renal problems, so patients with any kind of kidney problems should tell the staff before the scan is done.
-
Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. MRI can be used to measure the tumor’s size and to identify enlarged lymph nodes, which may indicate that cancer has spread. A special dye called a contrast medium is given before the scan to create a clearer picture. This dye is different from the one given for a CT scan (see above) and can be injected into a patient’s vein.
-
Bone scan. A bone scan uses a radioactive tracer to look at the inside of the bones. The amount of radiation in the tracer is too low to be harmful. The tracer is injected into a patient’s vein. It collects in areas of the bone and is detected by a special camera. Healthy bone appears lighter to the camera, and areas of injury, such as those caused by cancer, stand out on the image. A bone scan may be recommended if there are specific symptoms or particular laboratory findings.
-
Positron emission tomography (PET) or PET-CT scan. A PET scan is usually combined with a CT scan (see above), called a PET-CT scan . However, you may hear your doctor refer to this procedure just as a PET scan. A PET scan is a way to create pictures of organs and tissues inside the body. A small amount of a radioactive substance is injected into the patient’s body. This substance is taken up by cells that use the most energy. Because cancer tends to use energy actively, it absorbs more of the radioactive substance. However, the amount of radiation in the substance is too low to be harmful. A scanner then detects this substance to produce images of the inside of the body.
Ongoing research suggests that, in specific situations, a PET scan may possibly be better than a CT scan or MRI alone at helping to find bladder cancer that has spread. Despite this, PET scans are not considered standard imaging for bladder cancer and are not commonly used for this disease.
-
Ultrasound. An ultrasound uses sound waves to create a picture of the internal organs. It can help find out if the kidneys or ureters are blocked. This test does not require any type of contrast medium.
After diagnostic tests are done, your doctor will review the results with you. If the diagnosis is cancer, these results also help the doctor describe the cancer. This is called staging and grading.
The next section in this guide is Stages and Grades . It explains the systems doctors use to describe the extent of the disease and the way cancer cells look under a microscope. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Stages and Grades
ON THIS PAGE: You will learn about how doctors describe a cancer’s growth or spread, as well as the way the tumor cells look when viewed under a microscope. This is called the stage and grade. Use the menu to see other pages.
What is cancer staging?
Staging is a way of describing where the cancer is located, if or where it has invaded or spread, and whether it is affecting other parts of the body.
Doctors use diagnostic tests to find out the cancer’s stage, so staging may not be complete until all of the tests are finished. Knowing the stage helps the doctor recommend the best kind of treatment, and it can help predict a patient's prognosis, which is the chance of recovery. There are different stage descriptions for different types of cancer.
For bladder cancer, the stage is determined based on examining the sample removed during a transurethral resection of bladder tumor (TURBT; see Diagnosis ) and finding out whether the cancer has spread to other parts of the body.
This page provides detailed information about the system used to find the stage of bladder cancer and the stage groups for bladder cancer, such as stage II or stage IV.
-
TNM staging system
-
Stage groups for bladder cancer
-
Grade (G)
TNM staging system
One tool that doctors use to describe the stage is the TNM system. Doctors use the results from diagnostic tests and scans to answer these questions:
-
Tumor (T): How large is the primary tumor? Where is it located?
-
Node (N): Has the tumor spread to the lymph nodes? If so, where and how many?
-
Metastasis (M): Has the cancer spread to other parts of the body? If so, where and how much?
The results are combined to determine the stage of cancer for each person. There are 5 stages: stage 0 (zero) and stages I through IV (1 through 4). The stage provides a common way of describing the cancer, so doctors can work together to plan the best treatments.
Staging can be clinical or pathological. Clinical staging is based on the results of tests done before surgery, which may include history, physical examinations, imaging scans, and biopsies. Pathological staging is based on what is found based on the surgery itself (such as removal of the entire bladder), including the results of physical examinations, imaging scans, and biopsies. In general, pathological staging gives the health care team the most amount of information to make a prognosis.
Here are more details on each part of the TNM system for bladder cancer.
Tumor (T)
Using the TNM system, the "T" plus a letter and/or number (0 to 4) is used to describe the size and location of the tumor. Stages may also be divided into smaller groups that help describe the tumor in even more detail. If there is more than 1 tumor, the lowercase letter "m" (multiple) is added to the "T" stage category. If the “T” stage starts with a lowercase “c,” it means that the tumor was staged clinically. If it starts with a lowercase “p,” it means that the tumor was staged pathologically. If a patient’s tumor is removed, specific tumor stage information is listed below.
Bladder cancer
TX: The primary tumor cannot be evaluated.
T0 (T zero): There is no evidence of a primary tumor in the bladder.
Ta: This refers to noninvasive papillary carcinoma. This type of growth often is found on a small section of tissue that easily can be removed with TURBT.
Tis: This stage is carcinoma in situ (CIS) or a "flat tumor." This means that the cancer is only found on or near the surface of the bladder. The doctor may also call it non-muscle-invasive bladder cancer, superficial bladder cancer, or noninvasive flat carcinoma. This type of bladder cancer often comes back after treatment, usually as another noninvasive cancer in the bladder.
T1: The tumor has spread to the connective tissue (called the lamina propria) that separates the lining of the bladder from the muscles beneath, but it does not involve the bladder wall muscle.
T2: The tumor has spread to the muscle of the bladder wall.
-
T2a: The tumor has spread to the inner half of the muscle of the bladder wall, which may be called the superficial muscle.
-
T2b: The tumor has spread to the deep muscle of the bladder (the outer half of the muscle).
T3: The tumor has grown into the perivesical tissue (the fatty tissue that surrounds the bladder).
-
T3a: The tumor has grown into the perivesical tissue, as seen through a microscope.
-
T3b: The tumor has grown into the perivesical tissue macroscopically. This means that the tumor(s) is large enough to be seen during imaging tests or to be seen or felt by the doctor.
T4: The tumor has spread to any of the following: the abdominal wall, the pelvic wall, the prostate or seminal vesicle (the tubes that carry semen), or the uterus or vagina.
-
T4a: The tumor has spread to the prostate, seminal vesicles, uterus, or vagina. Surgical removal of the tumor may still be possible in this stage.
-
T4b: The tumor has spread to the pelvic wall or the abdominal wall. Surgical removal of the tumor may not be possible in this stage.
Renal pelvis and ureter
TX: The primary tumor cannot be evaluated.
T0 (T zero): There is no evidence of a primary tumor in the renal pelvis or ureter.
Ta: This refers to noninvasive papillary carcinoma. This type of growth often is found on a small section of tissue that easily can be removed with endoscopic resection.
Tis: This stage is carcinoma in situ (CIS) or a "flat tumor."
T1: The tumor has spread to the connective tissue beneath the lining of the renal pelvis or ureter.
T2: The tumor has spread to the muscle layer.
T3: The tumor has grown into the peripelvic fat (layers of fat around the kidney), into the renal parenchyma (the part of the kidney that filters blood and makes urine), or into the fat around the ureter.
T4: The tumor has spread to nearby organs or into the outer layer of fat on the kidney.
Node (N)
The “N” in the TNM staging system stands for lymph nodes. These small, bean-shaped organs help fight infection. Lymph nodes near where the cancer started, within the true pelvis (called hypogastric, obturator, iliac, perivesical, pelvic, sacral, and presacral lymph nodes), are called regional lymph nodes. Lymph nodes in other parts of the body are called distant lymph nodes.
Bladder cancer
NX: The regional lymph nodes cannot be evaluated.
N0 (N zero): The cancer has not spread to the regional lymph nodes.
N1: The cancer has spread to 1 regional lymph node in the pelvis.
N2: The cancer has spread to 2 or more regional lymph nodes in the pelvis.
N3: The cancer has spread to the common iliac lymph nodes, which are located behind the major arteries in the pelvis, above the bladder.
Renal pelvis and ureter
NX: The regional lymph nodes cannot be evaluated.
N0 (N zero): The cancer has not spread to the regional lymph nodes.
N1: The cancer is 2 centimeters (cm) or smaller in a single lymph node.
N2: The cancer is larger than 2 cm in a single lymph node, or it has spread to more than 1 lymph node.
Metastasis (M)
The "M" in the TNM system describes whether the cancer has spread to other parts of the body, called metastasis.
Bladder cancer
M0 (M zero): The disease has not metastasized.
M1: There is metastasis.
-
M1a: The cancer has spread only to lymph nodes outside of the pelvis.
-
M1b: The cancer has spread other parts of the body.
Renal pelvis and ureter
M0 (M zero): The disease has not metastasized.
M1: There is metastasis.
Return to top
Stage groups for bladder cancer
Doctors assign the stage of the bladder cancer by combining the T, N, and M classifications (see above).
Bladder cancer
Stage 0a: This is an early cancer that is only found on the surface of the inner lining of the bladder. Cancer cells are grouped together and can often be easily removed. The cancer has not invaded the muscle or connective tissue of the bladder wall. This type of bladder cancer is also called noninvasive papillary urothelial carcinoma (Ta, N0, M0).
Stage 0is: This stage of cancer, also known as a flat tumor or carcinoma in situ (CIS), is found only on the inner lining of the bladder. It has not grown in toward the hollow part of the bladder, and it has not spread to the thick layer of muscle or connective tissue of the bladder (Tis, N0, M0). This is always a high-grade cancer (see “Grades,” below) and is considered an aggressive disease because it can lead to muscle-invasive disease.
Stage I: The cancer has grown through the inner lining of the bladder and into the lamina propria. It has not spread to the thick layer of muscle in the bladder wall or to lymph nodes or other organs (T1, N0, M0).
Stage II: The cancer has spread into the thick muscle wall of the bladder. It is also called invasive cancer or muscle-invasive cancer. The tumor has not reached the fatty tissue surrounding the bladder and has not spread to the lymph nodes or other organs (T2, N0, M0).
Stage III: The cancer has spread throughout the muscle wall to the fatty layer of tissue surrounding the bladder (perivesical tissue) or to the prostate or the uterus and vagina. Or, the cancer has spread to the regional lymph nodes.
-
Stage IIIA: The tumor has grown into the perivesical tissue or has spread to the prostate, uterus, or vagina, but has not spread to the lymph nodes or other organs (T3a, T3b, or T4a; N0; M0). Or, the cancer has spread to a single regional lymph node (T1 to T4a, N1, M0).
-
Stage IIIB: The cancer has spread to 2 or more regional lymph nodes or to the common iliac lymph nodes (T1 to T4a, N2 or N3, M0).
Stage IV: The tumor has spread into the pelvic wall or abdominal wall, or the cancer has spread to lymph nodes outside of the pelvis or to other parts of the body.
-
Stage IVA: The tumor has spread to the pelvic wall or the abdominal wall but not to other parts of the body (T4b, any N, M0). Or, the cancer has spread to lymph nodes located outside of the pelvis (any T, any N, M1a).
-
Stage IVB: The cancer has spread other parts of the body (any T, any N, M1b).
Renal pelvis and ureter
Stage 0a: This is an early cancer that is only found on the surface of the inner lining of the renal pelvis or ureter. Cancer cells are grouped together and can often be easily removed. This type of cancer is also called noninvasive papillary carcinoma (Ta, N0, M0).
Stage 0is: This stage of cancer, also known as a flat tumor or carcinoma in situ (CIS), is found only on the inner lining of the renal pelvis or ureter (Tis, N0, M0).
Stage I: The cancer has grown into the inner lining of the renal pelvis or ureter. The cancer has not spread to the lymph nodes or other parts of the body (T1, N0, M0).
Stage II: The cancer has grown into the muscle behind the inner lining of the renal pelvis or ureter. The cancer has not spread to the lymph nodes or other parts of the body (T2, N0, M0).
Stage III: The cancer has grown past the muscle and into the fat surrounding the kidney or ureter or into the renal parenchyma. The cancer has not spread to the lymph nodes or other parts of the body (T3, N0, M0).
Stage IV: The tumor has invaded nearby organs or to the outer layer of fat of the kidney (T4, NX or N0, M0), or the cancer involves the lymph nodes (any T, N1 or N2, M0), or there is distant metastasis (any T, any N, M1).
Recurrent cancer
Recurrent cancer is cancer that has come back after treatment. If the cancer does return, there will be another round of tests to learn about the extent of the recurrence. These tests and scans are often similar to those done at the time of the original diagnosis .
Return to top
Grade (G)
Doctors also describe this type of cancer by its grade (G). The grade describes how much cancer cells look like healthy cells when viewed under a microscope.
The doctor compares the cancerous tissue with healthy tissue. Healthy tissue usually contains many different types of cells grouped together. If the cancer looks similar to healthy tissue and has different cell groupings, it is called "differentiated" or a "low-grade tumor." If the cancerous tissue looks very different from healthy tissue, it is called "poorly differentiated" or a "high-grade tumor."
Many urologic surgeons classify a tumor’s grade based on the chance that the cancer will recur or grow and spread, called progression. They often plan treatment based on the grade, using the following categories:
-
Low grade. This type of cancer may recur.
-
High grade. This type of cancer is more likely to recur and grow.
Return to top
Used with permission of the American College of Surgeons, Chicago, Illinois. The original and primary source for this information is the AJCC Cancer Staging Manual, Eighth Edition (2017), published by Springer International Publishing.
Doctors have different ways to treat bladder cancer. The next section in this guide is Types of Treatment . Use the menu to choose a different section to read in this guide.
Bladder Cancer - Types of Treatment
ON THIS PAGE: You will learn the basics about the different types of treatments doctors use for people with bladder cancer. Use the menu to see other pages.
This section explains the types of treatments, also known as therapies, that are the standard of care for cancer. “Standard of care” means the best treatments known so far. When making treatment plan decisions, you are encouraged to discuss with your doctor whether clinical trials are an option. A clinical trial is a research study that tests a new or modified approach to treatment. Doctors learn through clinical trials whether a new treatment is safe, effective, and possibly better than the standard treatment. Clinical trials can test a new drug, a new combination of standard treatments, or new doses of standard drugs or other treatments. Clinical trials are an option for all stages of cancer. Your doctor can help you consider all your treatment options, including clinical trials. Learn more about clinical trials in the About Clinical Trials and Latest Research sections of this guide.
How bladder cancer is treated
Different people with bladder cancer have different needs that have to treated. The treatments that your doctor recommends in the treatment plan are chosen based on the characteristics of your diagnosis and your overall health, as well as other factors.
Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Also, talk about the goals of each treatment with your doctor and what you can expect while receiving the treatment. These types of talks are called “shared decision-making.” Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision-making is particularly important for bladder cancer because there are different treatment options. Learn more about making treatment decisions .
To read an overview of treatment options based on the extent of the bladder cancer, read the next section in this guide, Treatments by Stage .
The most common types of treatments used for bladder cancer are described below. Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
-
Surgery
-
Chemotherapy
-
Immunotherapy
-
Targeted therapy
-
Gene therapy
-
Radiation therapy
-
Physical, social, and emotional effects of cancer
-
Remission and the chance of recurrence
-
If treatment does not work
Surgery
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. There are different types of surgery for bladder cancer. Your health care team will recommend a specific surgery based on the stage and grade of the disease.
Transurethral bladder tumor resection (TURBT).
This procedure is used for
diagnosis
and
staging
, as well as treatment. During TURBT, a surgeon inserts a cystoscope through the urethra into the bladder. The surgeon then removes the tumor using a tool with a small wire loop, a laser, or high-energy electricity, which is called fulguration. The patient is given an anesthetic, medication to block the awareness of pain, before the procedure begins.
For people with non-muscle-invasive bladder cancer, TURBT may be able to eliminate the cancer. However, the doctor may recommend additional treatments after TURBT to lower the risk of the cancer returning, such as intravesical chemotherapy or immunotherapy (see below).
For people with muscle-invasive bladder cancer, additional treatments involving surgery to remove the bladder or, less commonly, radiation therapy are usually recommended. Chemotherapy is commonly used in muscle-invasive bladder cancer.
Radical cystectomy and lymph node dissection. A radical cystectomy is the removal of the whole bladder and possibly nearby tissues and organs. These organs may include the prostate and part of the urethra or the uterus, fallopian tubes, ovaries, and part of the vagina.
For all patients, lymph nodes in the pelvis are removed. This is called a pelvic lymph node dissection. An extended pelvic lymph node dissection is the most accurate way to find cancer that has spread to the lymph nodes.
In rare, very specific situations, it might be appropriate to remove only part of the bladder, which is called partial cystectomy. However, this surgery is not the standard of care for people with muscle-invasive disease.
During a laparoscopic or robotic cystectomy, the surgeon makes several small incisions, or cuts, instead of the 1 larger incision used for traditional open surgery. The surgeon then uses telescoping equipment with or without robotic assistance to remove the bladder. The surgeon must make an incision to remove the bladder and surrounding tissue. This type of operation requires a surgeon who is very experienced in this type of surgery. Your doctor can discuss these options with you and help you make an informed decision.
Urinary diversion. If the entire bladder is removed, the doctor will create a new way to pass urine out of the body. One way to do this is to use a section of the small intestine or colon to divert urine to a stoma or ostomy (an opening) on the outside of the body. The patient then must wear a bag attached to the stoma to collect and drain urine.
Surgeons can sometimes use part of the small or large intestine to make a urinary reservoir, which is a storage pouch that sits inside the body. With these procedures, the patient does not need a urinary bag. For some patients, the surgeon is able to connect the pouch to the urethra, creating what is called an orthotopic neobladder, so the patient can pass urine out of the body. However, the patient may need to insert a thin tube called a catheter if the neobladder is not fully emptied of urine. Also, patients with a neobladder will no longer have the urge to urinate and will need to learn to urinate on a consistent schedule. For other patients, an internal (inside the abdomen) pouch made of small and/or large intestine is created and connected to the skin on the abdomen or belly button (umbilicus) through a small stoma (an example is an "Indiana Pouch"). With this approach, patients do not need to wear a bag. Patients drain the internal pouch multiple times a day by inserting a catheter through the small stoma and immediately removing the catheter. Your health care team will help you adapt to these changes.
Side effects of bladder cancer surgery
Living without a bladder can affect a person's quality of life. Finding ways to keep all or part of the bladder is an important treatment goal. For some people with muscle-invasive bladder cancer, treatment plans involving chemotherapy and radiation therapy after TURBT (see "Bladder preservation" in Treatments by Stage ) may be used as an alternative to removing the bladder.
The side effects of bladder cancer surgery depend on the procedure. Research has shown that having a surgeon with expertise in bladder cancer can improve the outcome of people with bladder cancer. Patients should talk with their doctor in detail to understand exactly what side effects may occur, including urinary and sexual side effects, and how they can be managed. In general, side effects may include:
-
Prolonged healing time
-
Infection
-
Blood clots or bleeding
-
Discomfort after surgery and injury to nearby organs
-
Infections or urine leaks after cystectomy or a urinary diversion. If a neobladder has been created, a patient may sometimes be unable to urinate or completely empty the bladder.
-
The inability of a penis to become erect, called erectile dysfunction , after cystectomy. Sometimes, a nerve-sparing cystectomy can be performed. When this is done successfully, a normal erection may be possible.
-
Damage to nerves in the pelvis and loss of sexual feeling and orgasm
-
Risks due to anesthesia or other coexisting medical issues
-
Loss of stamina or physical strength for some time
-
Change in the acid-base balance in the body and low levels of vitamin B12
Before surgery, talk with your health care team about the possible side effects from the specific surgery you will have. Learn more about the basics of cancer surgery .
Return to top
Therapies using medication
The treatment plan may include medications to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the cancer or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication.
Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for bladder cancer include:
-
Chemotherapy
-
Immunotherapy
-
Targeted therapy
-
Gene therapy
Each of these types of therapies is discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications prescribed for you, their purpose, and their potential side effects and interactions with other medications.
It is also important to let your doctor know if you are taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with cancer medications, causing unwanted side effects or reduced effectiveness. Learn more about your prescriptions by using searchable drug databases .
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells.
A chemotherapy regimen, or schedule, typically consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or a combination of different drugs given the same day.
There are 2 types of chemotherapy that may be used to treat bladder cancer. The type the doctor recommends and when it is given depends on the stage of the cancer. Talk with your doctor about chemotherapy before or after surgery.
-
Intravesical chemotherapy. Intravesical, or local, chemotherapy is usually given by a urologist. During this type of therapy, drugs are delivered into the bladder through a catheter that has been inserted through the urethra. Local treatment only destroys superficial tumor cells that come in contact with the chemotherapy solution. It cannot reach tumor cells in the bladder wall or tumor cells that have spread to other organs. Mitomycin-C (available as a generic drug), gemcitabine (Gemzar), docetaxel (Taxotere), and valrubicin (Valstar) are the drugs used most often for intravesical chemotherapy. The U.S. Food and Drug Administration (FDA) has also approved mitomycin (Jelmyto) for treatment of low-grade upper tract urothelial cancer.
-
Systemic chemotherapy. The most common regimens for systemic, or whole-body, chemotherapy to treat bladder cancer include:
-
Cisplatin and gemcitabine
-
Carboplatin (available as a generic drug) and gemcitabine
-
MVAC, which combines 4 drugs: methotrexate (Rheumatrex, Trexall), vinblastine (Velban), doxorubicin, and cisplatin
-
Dose-dense (DD)-MVAC with growth factor support: This is the same regimen as MVAC, but there is less time between treatments and has mostly replaced MVAC
-
Docetaxel or paclitaxel (available as a generic drug)
-
Pemetrexed (Alimta)
-
Many systemic chemotherapies continue to be tested in clinical trials to help find out which drugs or combinations of drugs work best to treat bladder cancer. Usually a combination of drugs works better than a single drug alone. Scientific evidence strongly supports the use of cisplatin-based chemotherapy before radical surgery for muscle-invasive bladder cancer. This is called neoadjuvant chemotherapy.
If platinum-based chemotherapy shrinks, slows, or stabilizes advanced or metastatic urothelial cancer, immunotherapy with avelumab (Bavencio, see "Immunotherapy" below) may be used to try to prevent or delay the cancer from coming back and to help people live longer. This is called switch maintenance treatment.
Side effects of chemotherapy depend on the individual drug, combination regimen, and the dose used, but they can include fatigue, risk of infection, blood clots and bleeding, loss of appetite, taste changes, nausea and vomiting, hair loss, and diarrhea, among others. These side effects usually go away after treatment is finished.
Learn more about the basics of chemotherapy .
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight cancer by improving your immune system’s ability to attack cancer cells. It can be given locally or throughout the body.
Local immunotherapy
Bacillus Calmette-Guerin (BCG). The standard immunotherapy drug for bladder cancer is a weakened mycobacterium called BCG, which is similar to the bacteria that causes tuberculosis. BCG is placed directly into the bladder through a catheter. This is called intravesical therapy. BCG attaches to the inside lining of the bladder and stimulates the immune system to destroy the tumor cells. BCG can cause flu-like symptoms, fevers, chills, fatigue, burning sensation in the bladder, and bleeding from the bladder, among others.
Interferon (Roferon-A, Intron A, Alferon). Interferon is another type of immunotherapy that may rarely be given as intravesical therapy. It is sometimes combined with BCG if using BCG alone does not help treat the cancer. Treatment with interferon is extremely uncommon nowadays.
Systemic immunotherapy
Immune checkpoint inhibitors ( updated 04/2023 ). An active area of immunotherapy research is looking at drugs that block PD-1 and PD-L1. PD-1 is found on the surface of T cells, which are a type of white blood cell that directly helps the body’s immune system fight disease. Because PD-1 keeps the immune system from destroying cancer cells, stopping PD-1 from working allows the immune system to better eliminate the cancer.
-
Avelumab (Bavencio). If chemotherapy has slowed or shrunk advanced urothelial cancer, the PD-L1 inhibitor avelumab can be given after chemotherapy, regardless of whether the tumor expresses PD-L1, since it has been shown to lengthen life and lower the risk of the cancer worsening. This kind of treatment is called switch maintenance therapy . Avelumab can also be used to treat advanced or metastatic urothelial carcinoma that has not been stopped by platinum chemotherapy.
-
Nivolumab (Opdivo). Nivolumab is a PD-1 inhibitor that can be used to treat advanced or metastatic urothelial carcinoma that has not been stopped by platinum chemotherapy. It may also be given after complete surgical removal of the cancer, called adjuvant therapy, to lower the chance of it coming back in people who are at high risk of recurrence based on cancer stage.
-
Pembrolizumab (Keytruda). Pembrolizumab is a PD-1 inhibitor that can be used to treat bladder cancer in these situations:
-
Advanced or metastatic urothelial carcinoma that has not been stopped by platinum chemotherapy. It is the only immunotherapy that has been shown to help people in this situation live longer (compared to taxane or vinflunine chemotherapy).
-
In combination with enfortumab vedotin for advanced or metastatic urothelial carcinoma among people who cannot receive cisplatin-based chemotherapy.
-
Non-muscle-invasive bladder cancer (Tis) that has not been stopped by BCG treatment in people who cannot receive or choose not to have radical cystectomy.
-
In the United States, people who cannot receive any platinum-based chemotherapy can receive pembrolizumab regardless of whether the tumor overexpresses PD-L1.
-
Immune checkpoint inhibitors continue to be studied in several clinical trials across all stages of bladder cancer.
Different types of immunotherapy can cause different side effects. Common side effects include fatigue, skin reactions (such as itching and rash), flu-like symptoms, thyroid gland function changes, hormonal and/or weight changes, diarrhea, and lung, liver, and gut inflammation, among others. Any body organ can be a target of an overactive immune system, so talk with your doctor about possible side effects for the immunotherapy recommended for you, so you know which changes to look for and can report them to the health care team early. Learn more about the basics of immunotherapy .
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and tries to limit damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your doctor may run genomic tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective standard treatment and relevant clinical trials whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of
targeted treatments
.
Erdafitinib (Balversa). Erdafitinib is a drug given by mouth (orally) that is approved to treat people with locally advanced or metastatic urothelial carcinoma with particular FGFR3 or FGFR2 genetic changes that has continued to grow or spread during or after platinum chemotherapy. There is a specific FDA-approved companion test to find out who may benefit from treatment with erdafitinib.
Common side effects of erdafitinib may include increased phosphate level, mouth sores, fatigue, nausea, diarrhea, dry mouth/skin, nails separating from the nail bed or poor nail formation, and change in appetite and taste, among others. Erdafitinib may also cause rare but serious eye problems, including retinopathy and epithelial detachment, which could cause blind spots that are called visual field defects. Evaluation by an ophthalmologist or optometrist is necessary at least every month in the first 4 months and then every 3 months after that time, along with frequent Amsler grid assessments at home.
Enfortumab vedotin-ejfv (Padcev) ( updated 04/2023 ). Enfortumab vedotin-ejfv is approved to treat locally advanced (unresectable) or metastatic urothelial cancer in:
-
People who have already received a PD-1 or PD-L1 immune checkpoint inhibitor (see “Immunotherapy,” above) and platinum-based chemotherapy
-
People who cannot receive cisplatin chemotherapy and have already received 1 or more treatments
-
Combination with pembrolizumab in people who cannot receive cisplatin-based chemotherapy.
Enfortumab vedotin-ejfv is an antibody-drug conjugate that targets Nectin-4, which is present in urothelial cancer cells. Antibody-drug conjugates attach to targets on cancer cells and then release a small amount of cancer medication directly into the tumor cells. Common side effects of enfortumab vedotin-ejfv include fatigue, peripheral neuropathy, rash, hair loss, changes in appetite and taste, nausea, diarrhea, dry eye, itching, dry skin, and elevated blood sugar, among others.
Sacituzumab govitecan (Trodelvy). Sacituzumab govitecan is approved to treat locally advanced or metastatic urothelial carcinoma that has previously been treated with a platinum-based chemotherapy and a PD-1 or PD-L1 immune checkpoint inhibitor, which applies to many people with urothelial carcinoma. Like enfortumab vedotin-ejfv, sacituzumab govitecan is an antibody-drug conjugate but has a very different structure, components, and mechanism of action. Common side effects of sacituzumab govitecan may include low count of certain white blood cells (neutropenia), nausea, diarrhea, fatigue, hair loss, anemia, vomiting, constipation, decreased appetite, rash, abdominal pain, and a few other, less common effects.
Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Return to top
Gene therapy ( updated 12/2022 )
Gene therapy is a treatment that alters the genetic code of cells to make them do something new or to improve certain functions. It can be used to train the body’s immune system to find and destroy cancer cells or to protect cells from the side effects of cancer treatment. Gene therapy may be offered to people with high-risk non-muscle-invasive bladder cancer, including carcinoma in situ, that has not responded to BCG treatment. Nadofaragene firadenovec (Adstiladrin) is gene therapy that uses a virus that is unable to replicate itself. The therapy is given by urinary catheter into the bladder. The virus includes a gene called IFN alpha2b . When the virus enters the cells lining the bladder, it releases the gene, and the gene becomes part of the genetic makeup of the bladder cells. This new gene teaches the cells to make the interferon alpha2b protein, and this protein helps destroy cancer cells. The most common side effects of nadofaragene firadenovec include bladder discharge, fatigue, bladder spasms, increased urge to urinate, blood in the urine, chills, fever, and pain when urinating.
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation therapy given from a machine outside the body. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
Radiation therapy is usually not used by itself as a primary treatment for bladder cancer, but it is typically given in combination with systemic chemotherapy. Some people who cannot receive chemotherapy might receive radiation therapy alone. Combined radiation therapy and chemotherapy may be used to treat cancer that is located only in the bladder:
-
To destroy any cancer cells that may remain after TURBT, so all or part of the bladder does not have to be removed, when appropriate (see "Bladder preservation" in Treatments by Stage ).
-
To relieve symptoms caused by a tumor, such as pain, bleeding, or blockage (called "palliative treatment," see section below).
Side effects from radiation therapy may include fatigue, mild skin reactions, and loose bowel movements. For bladder cancer, side effects most commonly occur in the pelvic or abdominal area and may include bladder irritation, with the need to pass urine frequently during the treatment period, and bleeding from the bladder or rectum; other side effects may occur less commonly. Most side effects tend to go away relatively soon after treatment is finished.
Learn more about the basics of radiation therapy .
Return to top
Physical, emotional, and social effects of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after an advanced cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your health care team may ask you to answer questions about your symptoms and side effects and to describe each problem. Be sure to tell the health care team if you are experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Return to top
Remission and the chance of recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. While many remissions are permanent, it is important to talk with your doctor about the possibility of the cancer returning. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence .
If the cancer returns after the original treatment, it is called recurrent cancer. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence, also known as metastasis).
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it. After this testing is done, you and your doctor will talk about the treatment options.
In general, non-muscle-invasive bladder cancers that come back in the same location as the original tumor or somewhere else in the bladder may be treated in a similar way as the first cancer. However, if the cancer continues to return after treatment, radical cystectomy may be recommended. Bladder cancers that recur outside the bladder are more difficult to eliminate with surgery and are often treated with systemic medications, radiation therapy, or both. Your doctor may also suggest clinical trials that are studying new ways to treat recurrent bladder cancer. Whichever treatment plan you choose, palliative care can be important for relieving symptoms and side effects.
People with recurrent cancer sometimes experience emotions such as disbelief or fear. You are encouraged to talk with your health care team about these feelings and ask about support services to help you cope. Learn more about dealing with cancer recurrence .
Return to top
If treatment does not work
Full recovery from bladder cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or metastatic.
This diagnosis is stressful, and for some people, advanced cancer is difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, expertise, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is a specific type of palliative care designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Learn more about advanced cancer care planning .
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss .
Return to top
Information about the cancer’s stage and grade will help the doctor recommend a specific treatment plan. The next section in this guide is Treatments by Stage . Use the menu to choose a different section to read in this guide.
Bladder Cancer - Treatments by Stage
ON THIS PAGE: You will learn about the general types of treatments doctors use to treat people with bladder cancer based on the stage of the disease. Use the menu to see other pages.
The information below outlines common types of treatment that may be part of your treatment plan, depending on the cancer’s stage (see Stages and Grades ). Please note that this is general information. Your doctor will recommend a personalized treatment plan for you based on the stage and other factors.
In general, the main treatment options for bladder cancer are:
-
Surgery
-
Chemotherapy
-
Immunotherapy (local and systemic)
-
Targeted therapy
-
Radiation therapy
To learn more about the basics of each type of treatment, read this guide’s Types of Treatment section.
Developing a treatment plan
In cancer care, different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team . This team is usually led by a urologist, a doctor who specializes in the genitourinary tract, or a urologic oncologist, a doctor who specializes in treating cancers of the genitourinary tract. Cancer care teams include a variety of other health care professionals, such as physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, and others.
Treatment options and recommendations depend on several factors, including:
-
The type, stage, and grade of bladder cancer
-
Possible side effects
-
The patient’s preferences and overall health
Your care plan also includes treatment for symptoms and side effects, an important part of cancer care.
The first treatment a person is given for advanced urothelial cancer is called first-line therapy. If that treatment stops working, then a person receives second-line therapy. In some situations, third-line therapy may also be available.
Adjuvant systemic therapy is treatment that is given after radical surgery has been completed. In bladder cancer, adjuvant therapy is usually cisplatin-based chemotherapy (if not given before surgery) or treatment in a clinical trial. Neoadjuvant therapy is treatment that is given before surgery, such as cisplatin-based chemotherapy.
The treatments your doctor recommends mainly depend on the stage of bladder cancer. Treatment for cancer in the renal pelvis and/or ureter follow the same treatment plans based on the stage of the disease. However, the tumor’s size and grade may also affect which treatment options are recommended for you. Talk with your doctor about the risks and benefits of all the available treatment options and when treatment should begin. Whichever treatment plan you choose, palliative care can be important for relieving symptoms and side effects (see “Physical, emotional, and social effects of cancer” in Types of Treatment ).
Treatments by type and stage of bladder cancer:
-
Noninvasive and non-muscle-invasive bladder cancer (stages 0a, 0is, and I)
-
Muscle-invasive bladder cancer (stage II and stage III)
-
Metastatic urothelial cancer (stage IV)
Noninvasive and non-muscle-invasive bladder cancer (stages 0a, 0is, and I) ( updated 12/2022 )
People with low-grade noninvasive bladder cancer (stage 0a) are treated with transurethral resection of bladder tumor (TURBT) first. Low-grade noninvasive bladder cancer rarely turns into aggressive, invasive, or metastatic disease, but patients are at risk for developing more low-grade cancers throughout their life. This requires long-term checkups, called surveillance, using cystoscopy and urine cytology (see Diagnosis ). To reduce the risk of future tumors developing, people may receive intravesical chemotherapy after TURBT.
Most commonly, people with high-grade noninvasive (stage Ta), carcinoma in situ (stage Tis), or non-muscle-invasive (stage T1) bladder cancer are treated with TURBT, followed by local intravesical Bacillus Calmette-Guerin (or BCG, see “Immunotherapy” in Types of Treatment ). This combination of treatments is given to reduce the risk of the cancer coming back, called recurrence, and the development of muscle-invasive disease. Before treatment with BCG, patients will need to have another TURBT to make sure that the cancer has not spread to the muscle. The first round of BCG treatment is given every week for 6 weeks. After that, the doctor performs a cystoscopy and sometimes a bladder biopsy (see Diagnosis ) to see if all of the cancer has been eliminated. If the cancer is gone, patients usually have maintenance therapy with BCG, which may be given once every 3 months for the first 6 months and then once every 6 months after that, for 1 to 3 years. This will then be followed with long-term surveillance.
People with high-grade, non-muscle-invasive bladder cancer are at higher risk for the tumor returning, called a recurrent tumor. Sometimes a tumor comes back at a more advanced stage, with a risk of developing into metastatic bladder cancer. To help prevent this from happening, the urologist may recommend removing the whole bladder, called radical cystectomy (see “Surgery” in Types of Treatment ), especially if the person is young, has a large tumor or a number of tumors at the time of diagnosis, or other aggressive features.
People with high-risk, non-muscle-invasive bladder cancer may also be treated with pembrolizumab or with gene therapy. Pembrolizumab is an immune checkpoint inhibitor that targets the PD-1 protein. Nadofaragene firadenovec is a gene therapy that is delivered into the bladder using a catheter. Both treatments are approved by the U.S. Food and Drug Administration (FDA) to treat bladder cancer that has not been stopped by, or responded to, BCG treatment (also called “BCG-unresponsive”) and radical cystectomy to remove the bladder cannot be done because of other medical reasons or the patient chooses not to have that surgery.
Return to top
Muscle-invasive bladder cancer (stage II and stage III)
Muscle-invasive bladder cancer has grown into the muscle layer of the bladder wall. Surgery is often among the first treatments, and the standard treatment is a radical cystectomy (see “Surgery” in Types of Treatment ). Lymph nodes near the bladder are usually removed as well. A TURBT may still be done, but it usually is used to help the doctor figure out the extent of the cancer rather than as a treatment. For some people, immunotherapy with nivolumab may be given after radical cystectomy with the goal of lowering the risk of recurrence.
Sometimes, people with muscle-invasive bladder cancer receive systemic chemotherapy first, before surgery. Then they may have a radical cystectomy and urinary diversion or may be given a combination of chemotherapy and radiation therapy. Giving neoadjuvant chemotherapy may shrink the tumor in the bladder, destroy microscopic cancer cells that have spread beyond the bladder, and ultimately help people live longer. An important clinical trial showed that a specific combination of systemic chemotherapy called MVAC given before radical cystectomy helped people with muscle-invasive bladder cancer live longer. This approach is now a standard treatment for people whose overall health allows it. The combination of 2 chemotherapy drugs, cisplatin and gemcitabine, is also considered a standard regimen for neoadjuvant therapy in muscle-invasive disease.
It is important to note that neoadjuvant chemotherapy should be a cisplatin-based combination. People whose health does not allow them to receive neoadjuvant cisplatin-based chemotherapy may receive radical surgery first or enroll in clinical trial. Anyone who has been diagnosed with muscle-invasive bladder cancer should talk with a urologist, a medical oncologist, and a radiation oncologist about all their treatment options, including the risks and benefits of radical surgery, chemotherapy, or radiation therapy, ideally in a multidisciplinary setting.
Bladder preservation
An approach using chemotherapy with radiation therapy after TURBT may provide the same benefits as removing the bladder. This is also known as the bladder preservation approach or trimodal therapy. The type of chemotherapy used for patients undergoing bladder radiation therapy can include cisplatin alone, gemcitabine alone, or a combination of mitomycin-C (available as a generic drug) and fluorouracil (5-FU). It is important to talk with your doctor about the difference between these 3 different chemotherapy regimens. Be sure to discuss the differences between surgery and bladder preservation approaches in detail, as well as all applicable clinical trials.
Return to top
Metastatic urothelial cancer (stage IV)
If bladder cancer has spread to another part of the body, doctors call it metastatic bladder cancer. If this happens, it is a good idea to talk with doctors, usually medical oncologists, who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Clinical trials may also be a good option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your chosen treatment plan.
A combination of treatments may be used to help manage the cancer. There are no methods to permanently cure metastatic urothelial cancer for most people. The goals of treatment are to slow the spread of cancer, delay its growth, shrink the tumor (called remission), and extend life for as long as possible. Palliative care is also important to help relieve cancer symptoms and treatment side effects.
Since there are relatively few treatment options for metastatic urothelial cancer, clinical trials are often the best treatment option for most people.
Chemotherapy. Currently, the standard first-line treatment options include chemotherapy regimens that contain cisplatin or carboplatin. These regimens include MVAC (rarely), dose-dense MVAC, and gemcitabine-cisplatin. Carboplatin regimens, such as with gemcitabine, can be used to treat people with metastatic urothelial cancer who cannot receive cisplatin. Chemotherapy with docetaxel or paclitaxel or pemetrexed are options for later-line treatment.
Immunotherapy ( updated 11/2022 ). Systemic immunotherapy has changed how metastatic urothelial cancer is managed. The FDA has approved several immune checkpoint inhibitors (see “Immunotherapy” in Types of Treatment ) for the treatment of people with metastatic disease. For example, pembrolizumab can be given as initial treatment in patients who may not be able tolerate chemotherapy. If platinum-based chemotherapy has stopped the cancer from growing, switch maintenance therapy with avelumab has been shown to help people live longer and reduce the risk of the cancer worsening. Pembrolizumab was shown to help people live longer if cancer grew again (worsened) after platinum-based chemotherapy. People are strongly encouraged to talk with their doctors about whether immunotherapy is right for them. Changes to these regimens or the use of new treatment regimens are being studied in many clinical trials, aiming at helping people live longer, lower the risk of recurrence, and improve quality of life.
Targeted therapy ( updated 04/2023 ). Erdafitinib may be used to treat people with locally advanced or metastatic urothelial carcinoma after platinum chemotherapy did not stop the cancer growth. Erdafitinib is a targeted therapy aimed at particular DNA changes in the FGFR2 or FGFR3 genes. Patients must have their tumor tested for these changes to be able to receive the treatment. Enfortumab vedotin-ejfv (Padcev), an antibody-drug conjugate, is also approved to be used alone to treat locally advanced (unresectable) or metastatic urothelial carcinoma in people who have also received a PD-1 or PD-L1 immune checkpoint inhibitor and platinum-based chemotherapy, as well as for those who cannot receive cisplatin-based chemotherapy and have already received 1 or more treatments. For those who cannot receive cisplatin-based chemotherapy, enfortumab vedotin in combination with pembrolizumab is an option. Another antibody-drug conjugate, sacituzumab govitecan, is approved to treat locally advanced or metastatic urothelial carcinoma that has previously been treated with a platinum-based chemotherapy and a PD-1 or PD-L1 immune checkpoint inhibitor. Learn more in the “Therapies using medication” section in Types of Treatment .
For many people, a diagnosis of metastatic cancer is very stressful and difficult. You and your family are encouraged to talk about how you feel with doctors, nurses, social workers, or other members of the health care team. It may also be helpful to talk with other patients, such as through a support group or other peer support program.
Return to top
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for people with cancer. Use the menu to choose a different section to read in this guide.
Bladder Cancer - About Clinical Trials
ON THIS PAGE: You will learn more about clinical trials, which are the main way that new medical approaches are studied to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to treat people with bladder cancer. To make scientific advances, doctors create research studies involving volunteers, called clinical trials. Every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials. Clinical trials are essential for developing new drugs and treatments.
Clinical trials are used for all types and stages of bladder cancer. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of treatments, new approaches to radiation therapy or surgery, and new methods of diagnosis or treatment.
People who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and the chance that the new treatment may not work as well. People are strongly encouraged to talk with their health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others aim to manage the late effects that may happen a long time after treatment. Talk with your doctor about clinical trials for symptoms and side effects.
Deciding to join a clinical trial
People decide to participate in clinical trials for many reasons. For some, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the uncertainty of a clinical trial in the hope and possibility of a better result. Others volunteer for clinical trials because they know that these studies are a great way to contribute to the progress in treating bladder cancer. Even if they may not benefit directly from the clinical trial, their participation can benefit future people with cancer.
Insurance coverage and the costs of clinical trials differ by location and by study. In a number of programs, some of the expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team and your insurance company first to learn if and how your treatment in a clinical trial will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, they may receive no treatment by being given a placebo or a “sugar pill.” When used, placebos are usually combined with standard treatment in most cancer clinical trials or when there is no available standard regimen. Study participants will always be told when a placebo is used in a study. Find out more about placebos in cancer clinical trials .
Patient safety and informed consent
To join a clinical trial, people must participate in a process known as informed consent. During informed consent, the doctor should:
-
Describe all of the treatment options, so that the person understands how the new treatment differs from the standard treatment.
-
List all of the risks of the new treatment, which may or may not be different from the risks of standard treatment.
-
Explain what will be required of each person in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
-
Describe the purposes of the clinical trial and what researchers are trying to learn.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together. You will need to meet all of the eligibility criteria in order to participate in a clinical trial. Learn more about eligibility criteria in clinical trials.
People who participate in a clinical trial may stop participating at any time for personal or medical reasons. This may include that the new treatment is not working or there are serious side effects. Clinical trials are also closely monitored by experts who watch for any problems with each study. It is important that people participating in a clinical trial talk with their doctor and researchers about who will be providing their treatment and care during the clinical trial, after the clinical trial ends, and/or if they choose to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of cancer. For specific topics being studied for bladder cancer, learn more in the Latest Research section.
Cancer.Net offers more information about cancer clinical trials in other areas of the website, including a complete section on clinical trials and places to search for clinical trials for a specific type of cancer . You may also find a list of clinical trials in bladder cancer on the website of the Bladder Cancer Advocacy Network (BCAN) . (Please note that this link takes to you a different website.)
In addition, you can find a free video-based educational program about cancer clinical trials in another section of this website.
The next section in this guide is Latest Research . It explains areas of scientific research for bladder cancer. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Latest Research
ON THIS PAGE: You will read about the scientific research being done to learn more about bladder cancer and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about bladder cancer, ways to prevent it, how to best treat it, and how to provide the best care to people diagnosed with this disease. The following areas of research may include new options for patients through clinical trials. Always talk with your doctor about the diagnostic and treatment options best for you.
-
Minimally invasive cystectomy. Several studies are exploring whether laparoscopic or robotic bladder removal is as safe and effective as standard surgery. Learn more about this type of surgery in the Types of Treatment section.
-
Expanding the use of bladder preservation. Researchers are actively looking at ways to help more people with bladder cancer keep their bladder, if possible, using treatments other than bladder removal.
-
Lymph node dissection. A study sponsored by the Southwest Oncology Group (SWOG) is looking at whether removing more lymph nodes than is standard practice, called extended lymph node dissection, can improve a patient’s prognosis and outcome.
-
Molecular tumor testing. Tests to identify changes to genes or proteins that could be a sign of bladder cancer may help predict a bladder cancer recurrence or predict which patients may need more intense treatment. DNA changes may also help predict prognosis for people with bladder cancer. Tumor genetics are becoming more and more important for the treatment of people with bladder cancer because test results may help doctors choose the best treatment options. Which new treatments are available depends on the genetic changes found in the tumor (see “Targeted therapy” below).
Studies have shown that certain inherited genetic traits can contribute to cancer development in some people. Therefore, it is very important to talk with your relatives about your broader family history of cancer and discuss with your doctors whether genetic counseling is recommended. This can help you and your family make decisions about treatment and cancer prevention.
-
Targeted therapy. Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells. Research is underway to find out how targeted therapy may be used to treat this cancer, and currently 3 drugs of this type are approved to treat metastatic urothelial cancer, as described in Types of Treatment . Additionally, clinical trials are looking at combining targeted therapy with other treatments. Learn more about the basics of targeted therapy .
-
Immunotherapy. Immunotherapy, also called biologic therapy, is designed to boost the body's natural defenses to fight the cancer. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function. An active area of immunotherapy research is looking at drugs called immune checkpoint inhibitors to treat advanced cancer. These drugs block proteins called PD-1, PD-L1, and CTLA-4. These proteins are found on the surface of T cells, which are a type of white blood cell that directly helps the body’s immune system fight disease. Because PD-1, PD-L1, and CTLA-4 keep the immune system from destroying cancer cells, stopping them from working allows the immune system to better eliminate the disease. Several drugs that block the PD-1/PD-L1 pathway have received U.S. Food and Drug Administration (FDA) approval to treat bladder cancer (see Types of Treatment ). Other research is underway in this area. Learn more about the basics of immunotherapy .
-
New drug combinations. Researchers are studying new combinations of chemotherapies and other medications to see if they are safe and more effective than other treatments.
-
Palliative care/supportive care. Clinical trials are underway to find a better way of reducing symptoms and side effects of current treatments to improve comfort and quality of life for patients.
Looking for More About the Latest Research?
If you would like additional information about the latest areas of research regarding bladder cancer, explore these related items:
-
To find clinical trials specific to your diagnosis, talk with your doctor or search online clinical trial databases .
-
Visit the Cancer.Net Blog to read about recent research in bladder cancer and to listen to podcasts with expert perspectives on the topic.
-
Visit the website of Conquer Cancer, the ASCO Foundation , to find out how to help support cancer research. Please note that this link takes you to a different ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance on how to cope with the physical, emotional, social, and financial changes that cancer and its treatment can bring. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Coping with Treatment
ON THIS PAGE: You will learn more about coping with the physical, emotional, social, and financial effects of cancer and its treatment. Use the menu to see other pages.
Every cancer treatment can cause side effects or changes to your body and how you feel. For many reasons, people do not experience the same side effects even when they are given the same treatment for the same type of cancer. This can make it hard to predict how you will feel during treatment.
As you prepare to start cancer treatment, it is normal to fear treatment-related side effects . It may help to know that your health care team will work to prevent and relieve side effects. This part of cancer treatment is called palliative care or supportive care. It is an important part of your treatment plan, regardless of your age or the stage of disease.
Coping with physical side effects
Common physical side effects from each treatment option for bladder cancer are described in the Types of Treatment section. Learn more about side effects of cancer and its treatment, along with ways to prevent or control them . Changes to your physical health depend on several factors, including the cancer’s stage, the length and dose of treatment, nutritional status, and your general health.
Talk with your health care team regularly about how you are feeling. It is important to let them know about any new side effects or changes in existing side effects. If they know how you are feeling, they can find ways to relieve or manage your side effects to help you feel more comfortable and potentially keep any side effects from worsening.
You may find it helpful to keep track of your side effects so it is easier to talk about any changes with your health care team. Learn more about why tracking side effects is helpful .
Sometimes, side effects can last after treatment ends. Doctors call these long-term side effects. Side effects that occur months or years after treatment are called late effects . Treating long-term side effects and late effects is an important part of survivorship care. Learn more by reading the Follow-up Care section of this guide or talking with your doctor.
Coping with emotional and social effects
You can have emotional and social effects after a cancer diagnosis. This may include dealing with a variety of emotions, such as sadness, anxiety, or anger, or managing your stress level. Sometimes, people find it difficult to express how they feel to their loved ones. Some have found that talking to an oncology social worker, counselor, or member of the clergy can help them develop more effective ways of coping and talking about cancer.
You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your needs.
Coping with the costs of cancer care
Cancer treatment can be expensive. It may be a source of stress and anxiety for people with cancer and their families. In addition to treatment costs, many people find they have extra, unplanned expenses related to their care. For some people, the high cost of medical care stops them from following or completing their cancer treatment plan. This can put their health at risk and may lead to higher costs in the future. Patients and their families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations in a separate part of this website.
Coping with barriers to care
Some groups of people experience different rates of new cancer cases and experience different outcomes from their cancer diagnosis. These differences are called “cancer disparities.” Disparities are caused in part by real-world barriers to quality medical care and social determinants of health , such as where a person lives and whether they have access to food and health care. Cancer disparities more often negatively affect racial and ethnic minorities , people with fewer financial resources , sexual and gender minorities (LGBTQ+) , adolescent and young adult populations , older adults , and people who live in rural areas or other underserved communities .
If you are having difficulty getting the care you need, talk with a member of your health care team or explore other resources that help support medically underserved people .
Talking with your health care team about side effects
Before starting treatment, talk with your doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they likely to happen?
-
What can we do to prevent or relieve them?
-
When and who should we call about side effects?
Be sure to tell your health care team about any side effects that happen during treatment and afterward, too. Tell them even if you do not think the side effects are serious. This discussion should include physical, emotional, social, and financial effects of cancer.
Caring for a loved one with cancer
Family members and friends often play an important role in taking care of a person with bladder cancer. This is called being a caregiver. Caregivers can provide physical, practical, and emotional support to the patient, even if they live far away. Being a caregiver can also be stressful and emotionally challenging. One of the most important tasks for caregivers is caring for themselves .
Caregivers may have a range of responsibilities on a daily or as-needed basis, including:
-
Providing support and encouragement
-
Talking with the health care team
-
Giving medications
-
Helping manage symptoms and side effects
-
Coordinating medical appointments
-
Providing a ride to and from appointments
-
Assisting with meals
-
Helping with household chores
-
Handling insurance and billing issues
A caregiving plan can help caregivers stay organized and help identify opportunities to delegate tasks to others. It may be helpful to ask the health care team how much care will be needed at home and with daily tasks during and after treatment. Use this 1-page fact sheet to help make a caregiving action plan. This free fact sheet is available as a PDF, so it is easy to print.
Learn more about caregiving or read the ASCO Answers Guide to Caring for a Loved One With Cancer in English or Spanish .
Looking for More on How to Track Side Effects?
Cancer.Net offers several resources to help you keep track of your symptoms and side effects. Please note that these links will take you to other sections of Cancer.Net:
-
Cancer.Net Mobile: The free Cancer.Net mobile app allows you to securely record the time and severity of symptoms and side effects.
-
ASCO Answers Managing Pain: Get this 32-page booklet about the importance of pain relief that includes a pain tracking sheet to help patients record how pain affects them. The free booklet is available as a PDF, so it is easy to print.
-
ASCO Answers Fact Sheets: Read 1-page fact sheets on anxiety and depression , constipation , diarrhea , rash , and immunotherapy side effects that provide a tracking sheet to record details about the side effect. These free fact sheets are available as a PDF, so they are easy to print, fill out, and give to your health care team.
The next section in this guide is Follow-up Care . It explains the importance of checkups after you finish cancer treatment. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Follow-Up Care
ON THIS PAGE: You will read about your medical care after cancer treatment is finished and why this follow-up care is important. Use the menu to see other pages.
Care for people diagnosed with bladder cancer does not end when active treatment has finished. Your health care team will continue to check that the cancer has not come back, manage any side effects, and monitor your overall health. This is called follow-up care and active monitoring.
Your follow-up care may include regular physical examinations, medical tests, or both. Doctors want to keep track of your recovery in the months and years ahead. For people treated for bladder cancer, follow-up care typically includes a general physical examination, cystoscopy (if the bladder has not been removed), urine cytology, type of x-rays, and routine blood and urine tests to make sure the bladder is working well and to check for any signs that the cancer has come back.
For people with a urinary diversion, follow-up care may include checking for infection with urine tests, checking and fixing problems with controlling urination, checking for recurrent cancer in the upper urinary tract, and checking for changes in kidney function with blood and urine tests and x-rays.
Tell your doctor about any new symptoms, such as pain during urination, blood in the urine, frequent urination, an immediate need to urinate, and any other symptoms. These symptoms may be signs that the cancer has come back or signs of another medical condition.
Cancer rehabilitation and survivorship care are often recommended, and this could mean any of a wide range of services, such as physical therapy, occupational therapy, career counseling, pain management, nutritional planning, financial counseling, and/or emotional counseling. The goal of rehabilitation is to help people regain control over many aspects of their lives and remain as independent as possible. Learn more about cancer rehabilitation.
Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence, which means that the cancer has come back. Cancer recurs because small areas of cancer cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms. During follow-up care, a doctor familiar with your medical history can give you personalized information about your risk of recurrence.
The anticipation before having a follow-up test or waiting for test results may add stress to you or a family member. This is sometimes called “scanxiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects
Most people expect to have side effects when receiving treatment. However, it is often surprising to survivors that some side effects may linger beyond the treatment period. These are called long-term side effects. Other side effects called late effects may develop months or even years after treatment has ended. Long-term and late effects can include both physical and emotional changes.
Talk with your doctor about your risk of developing such side effects based on your diagnosis, your individual treatment plan, and your overall health. If you had a treatment known to cause specific late effects, you may have certain physical examinations, scans, or blood tests to help find and manage them.
Keeping personal health records
You and your doctor should work together to develop a personalized follow-up care plan. Be sure to discuss any concerns you have about your future physical or emotional health. ASCO offers forms to help keep track of the cancer treatment you received and develop a survivorship care plan when treatment is completed.
This is also a good time to talk with your doctor about who will lead your follow-up care. Some survivors continue to see their oncologist or urologist, while others transition back to the care of their primary care doctor or another health care professional. This decision depends on several factors, including the type and stage of bladder cancer, side effects, health insurance rules, and your personal preferences, expectations, and beliefs.
If a doctor who was not directly involved in your cancer care will lead your follow-up care, be sure to share your cancer treatment summary and survivorship care plan forms with them and with all future health care providers. Details about your cancer treatment and communication preferences are very valuable to the health care professionals who will care for you throughout your lifetime.
The next section in this guide is Survivorship . It describes how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Survivorship
ON THIS PAGE: You will read about how to cope with challenges in everyday life after a cancer diagnosis. Use the menu to see other pages.
What is survivorship?
The word “survivorship” is complicated because it means different things to different people. Common definitions include:
-
Having no signs of cancer after finishing treatment.
-
Living with, through, and beyond cancer. According to this definition, cancer survivorship begins at diagnosis and continues during treatment and through the rest of a person's life.
For some, even the term “survivorship” does not feel right, and they prefer to use different language to describe and define their experience. Sometimes extended treatment will be used for months or years to manage or control cancer. Living with cancer indefinitely is not easy, and the health care team can help you manage the challenges that come with it . Everyone has to find their own path to name and navigate the changes and challenges that are the results of their cancer diagnosis and treatment.
Survivors may experience a mixture of feelings, including joy, concern, relief, guilt, and fear. Some people say they appreciate life more after a cancer diagnosis and have gained a greater acceptance of themselves. Others become very anxious about their health and uncertain about coping with everyday life. Feelings of fear and anxiety may still occur as time passes, but these emotions should not be a constant part of your daily life. If they persist, be sure to talk with a member of your health care team.
Survivors may feel some stress when their frequent visits to the health care team end after completing treatment. Often, relationships built with the cancer care team provide a sense of security during treatment, and people miss this source of support. This may be especially true when new worries and challenges surface over time, such as any late effects of treatment, emotional challenges including fear of recurrence, sexual health and fertility concerns, and financial and workplace issues.
Every survivor has individual concerns and challenges. With any challenge, a good first step is being able to recognize your fears and talk about them. Effective coping requires:
-
Understanding the challenge you are facing
-
Thinking through solutions
-
Asking for and allowing the support of others
-
Feeling comfortable with the course of action you choose
Many survivors find it helpful to join an in-person support group or an online community of survivors. This allows you to talk with people who have had similar first-hand experiences. Other options for finding support include talking with a friend or member of your health care team, individual counseling, or asking for assistance at the learning resource center of the place where you received treatment.
A new perspective on your health
For many people, survivorship serves as a strong motivator to make lifestyle changes.
People recovering from bladder cancer are encouraged to follow established guidelines for good health, such as not smoking, limiting alcohol, eating well, exercising regularly, and managing stress. Regular physical activity can help rebuild your strength and energy level. Your health care team can help you create an appropriate exercise plan based upon your needs, physical abilities, and fitness level. Learn more about making healthy lifestyle choices .
It is important to have recommended medical checkups and tests (see Follow-up Care ) to take care of your health.
Talk with your health care team to develop a survivorship care plan that is best for your needs.
Changing role of caregivers
Family members and friends may also go through periods of transition. A caregiver plays a very important role in supporting a person diagnosed with cancer, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver's role often changes. Eventually, the need for caregiving related to the cancer diagnosis will become much less or come to an end. Caregivers can learn more about adjusting to life after caregiving .
Looking for More Survivorship Resources?
For more information about cancer survivorship, explore these related items. Please note that these links will take you to other sections of Cancer.Net:
-
ASCO Answers Guide to Cancer Survivorship: Get this 48-page booklet that helps people transition into life after treatment. It includes blank treatment summary and survivorship care plan forms. The free booklet is available as a PDF, so it is easy to print.
-
Survivorship Resources: Cancer.Net offers information and resources to help survivors cope, including specific sections for children , teens and young adults , and people over age 65 . There is also a main section on survivorship for people of all ages.
The next section offers Questions to Ask the Health Care Team to help start conversations with your cancer care team. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Questions to Ask The Health Care Team
ON THIS PAGE: You will find some questions to ask your doctor or other members of the health care team to help you better understand your diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with the health care team is important to make informed decisions about your health care. These suggested questions are a starting point to help you learn more about your cancer care and treatment. You are also encouraged to ask additional questions that are important to you. You may want to print this list and bring it to your next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your care. It may also be helpful to ask a family member or friend to come with you to appointments to help take notes.
Questions to ask after getting a diagnosis
-
What type of bladder cancer do I have?
-
Is it non-invasive or invasive? What does this mean?
-
If the cancer is invasive, does it involve the muscle?
-
Can you explain my pathology report (laboratory test results) to me?
-
What is the stage of my cancer? What does this mean?
-
What is the grade? What does this mean?
-
Should I seek a second opinion?
-
Should I seek genetic counseling and/or testing?
Questions to ask about choosing a treatment and managing side effects
-
How soon do I need to start treatment?
-
What are my treatment options?
-
What clinical trials are available for me? Where are they located, and how do I find out more about them?
-
What treatment plan do you recommend? Why?
-
What is the goal of each treatment? Is it to eliminate the cancer, help me feel better, or both?
-
What are the possible side effects of each treatment, both in the short term and the long term?
-
Who will be part of my health care team, and what does each member do?
-
Who will be leading my overall treatment?
-
How will this treatment affect my daily life? Will I be able to work, exercise, and perform my usual activities?
-
Could this treatment affect my sex life? If so, how and for how long? How can sexual side effects that occur be managed?
-
Could this treatment affect my ability to become pregnant or have children? If so, should I talk with a fertility specialist before cancer treatment begins?
-
If I’m worried about managing the costs of cancer care, who can help me?
-
If I have questions or problems, who should I call?
Questions to ask about having surgery
-
What type of surgery will I have?
-
How many procedures of this type has the surgeon done?
-
Will my entire bladder be removed?
-
Do you have experience making urinary reservoirs? Can I have this type of surgery?
-
How long will the operation take?
-
How long will I be in the hospital?
-
Can you describe what my recovery from surgery will be like?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term side effects of having this surgery?
-
How will the surgery affect my ability to urinate?
-
Will I need to use a catheter?
-
Will I need to have a urostomy ? If so, how do I care for my urostomy?
-
If I have a neobladder, how will I know when I need to empty it?
Questions to ask about having therapy using medications
-
What type of medication do you recommend?
-
What is the goal of this treatment?
-
How will it be delivered? Through an IV, a catheter, or a pill?
-
How long will it take to give this treatment?
-
Will I receive this treatment at a hospital or clinic? Or will I take it at home?
-
How can I prepare for this treatment?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of this type of chemotherapy?
-
What can be done to prevent or manage these side effects?
Questions to ask about having radiation therapy
-
What type of radiation therapy do you recommended?
-
What is the goal of radiation therapy?
-
How long will it take to give radiation therapy?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects I experience? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or manage these side effects?
Questions to ask about planning follow-up care
-
What is the chance that the cancer will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the cancer treatment I received?
-
What follow-up tests will I need, and how often will those tests be needed?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
Who will be leading my follow-up care?
-
What survivorship support services are available to me? To my family?
The next section in this guide is Additional Resources . It offers more resources on this website that may be helpful to you. Use the menu to choose a different section to read in this guide.
Bladder Cancer - Additional Resources
ON THIS PAGE: You will find some helpful links to other areas of Cancer.Net that provide information about cancer care and treatment. This is the final page of Cancer.Net’s Guide to Bladder Cancer. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of cancer for the person diagnosed and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Here are a few links to help you explore other parts of Cancer.Net:
-
Search for a cancer specialist in your local area using this free database of doctors from the American Society of Clinical Oncology.
-
Learn what medical phrases and terms used in cancer care and treatment mean.
-
Read more about the first steps to take when you are diagnosed with cancer .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of cancer care.
-
Learn more about coping with the emotions that cancer can bring, including those within a family or a relationship.
-
Find a national, not-for-profit advocacy organization that may offer additional information, services, and support for people with bladder cancer.
-
Explore what to do when you finish active treatment .
-
Download Cancer.Net Mobile , a free app that includes a symptom and side effect tracker, medication reminders, and other interactive resources.
-
To find a range of information and insights from different voices on timely cancer topics, visit the Cancer.Net Blog .
-
Watch Cancer.Net videos with ASCO experts explaining the basics of cancer treatment, side effects, survivorship, clinical trials, caregiving, and more.
-
For more information about treatment options for this disease, see the following topic review from UpToDate: Patient information: Bladder cancer treatment; invasive cancer (Beyond the Basics) . Please note that this link takes you to a separate, independent website.
This is the end of Cancer.Net’s Guide to Bladder Cancer. Use the menu to choose a different section to read in this guide.













