Astrocytoma - Childhood - Introduction
ON THIS PAGE: You will find some basic information about astrocytoma and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Childhood Astrocytoma. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
The brain and spinal column make up the central nervous system (CNS). The CNS controls all vital functions of the body, including thought, speech, and strength.
Astrocytoma is a type of CNS tumor that forms in cells called astrocytes. Healthy astrocytes provide the connecting network of the brain and spinal cord. When the CNS is damaged, astrocytes form scar tissue. Astrocytoma begins when healthy astrocytes change and grow out of control, forming a mass called a tumor.
Astrocytoma can occur throughout the CNS, including in the following places:
-
The cerebellum , which is the back part of the brain responsible for coordination and balance
-
The cerebrum , which is the top part of the brain that controls motor activities and talking
-
The diencephalon , which is the central part of the brain that controls vision, hormone production, and arm and leg movement
-
The brain stem , which controls eye and facial movement, arm and leg movement, and breathing
-
The spinal cord, which controls sensation and arm and leg motor function
In general, a tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but spread is very rare. Astrocytoma is more commonly referred to as either high grade or low grade (see Stages and Grades ).

Normal brain tissue

Pilocytic astrocytoma (low-grade tumor)

Anaplastic astrocytoma (high-grade tumor)
These images are used with permission by the College of American Pathologists.
This section covers astrocytoma diagnosed in children. Learn more about brain tumors in adults in a separate guide on this same website.
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
Cancer.Net Patient Education Video: View a short video led by an ASCO expert in brain tumors that provides basic information and areas of research.
-
Cancer.Net En Español: Read about astrocytoma in Spanish. Infórmase sobre astrocitoma en español .
The next section in this guide is Statistics . It helps explain the number of children who are diagnosed with astrocytoma and general survival rates. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Statistics
ON THIS PAGE: You will find information about the estimated number of children and teens who will be diagnosed with astrocytoma each year. You will also read general information on surviving the disease. Remember, survival rates depend on several factors, and no 2 people with a tumor are the same. Use the menu to see other pages.
Every person is different, with different factors influencing their risk of being diagnosed with this tumor and the chance of recovery after a diagnosis. It is important to talk with your doctor about any questions you have around the general statistics provided below and what they may mean for your child individually. The original sources for these statistics are provided at the bottom of this page.
How many children and teens are diagnosed with astrocytoma?
Astrocytoma accounts for about half of all brain tumors in children. In 2023, an estimated 1,118 children and teens age 0 to 19 in the United States will be diagnosed with astrocytoma. Pilocytic astrocytomas make up an estimated 15% of all brain and other central nervous system (CNS) tumors in this age group.
What is the survival rate for astrocytoma?
There are different types of statistics that can help doctors evaluate a child or teen’s chance of recovery from astrocytoma. These are called survival statistics. A specific type of survival statistic is called the relative survival rate. It is often used to predict how having a tumor may affect life expectancy. Relative survival rate looks at how likely people with astrocytoma are to survive for a certain amount of time after their initial diagnosis or start of treatment compared to the expected survival of similar people without this tumor.
Example: Here is an example to help explain what a relative survival rate means. Please note this is only an example and not specific to this type of cancer. Let’s assume that the 5-year relative survival rate for a specific type of cancer is 90%. “Percent” means how many out of 100. Imagine there are 1,000 people without cancer, and based on their age and other characteristics, you expect 900 of the 1,000 to be alive in 5 years. Also imagine there are another 1,000 people similar in age and other characteristics as the first 1,000, but they all have the specific type of cancer that has a 5-year survival rate of 90%. This means it is expected that 810 of the people with the specific cancer (90% of 900) will be alive in 5 years.
It is important to remember that statistics on the survival rates for children and teens with astrocytoma are only an estimate. They cannot tell an individual person if the tumor will or will not shorten their life. Instead, these statistics describe trends in groups of people previously diagnosed with the same disease, including specific stages of the disease.
For children younger than 15, the 5-year relative survival rate for pilocytic astrocytoma is 97%. For those with diffuse astrocytoma, the 5-year relative survival rate is 82%. The 5-year relative survival rate for anaplastic astrocytoma is 25%.
The survival rates for astrocytoma vary based on several factors. These include the stage of tumor, a person’s age and general health, and how well the treatment plan works. Other factors that can affect outcomes include the grade of the astrocytoma and how much of the tumor can be removed during surgery. Children and teens with a type of astrocytoma that is unlikely to spread, called noninfiltrating astrocytoma, generally have a higher 5-year relative survival rate.
Experts measure relative survival rate statistics for astrocytoma every 5 years. This means the estimate may not reflect the results of advancements in how astrocytoma is diagnosed or treated from the last 5 years. Talk with your child’s doctor if you have any questions about this information. Learn more about understanding statistics .
Statistics adapted from the Central Brain Tumor Registry of the United States Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2015–2019, published October 2022, and the Children’s Oncology Group CureSearch for Children’s Cancer website. (All sources accessed February 2023.)
The next section in this guide is Medical Illustrations . It offers drawings of body parts often affected by astrocytoma. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Medical Illustrations
ON THIS PAGE: You will find drawings of the main body parts affected by astrocytoma. Use the menu to see other pages.
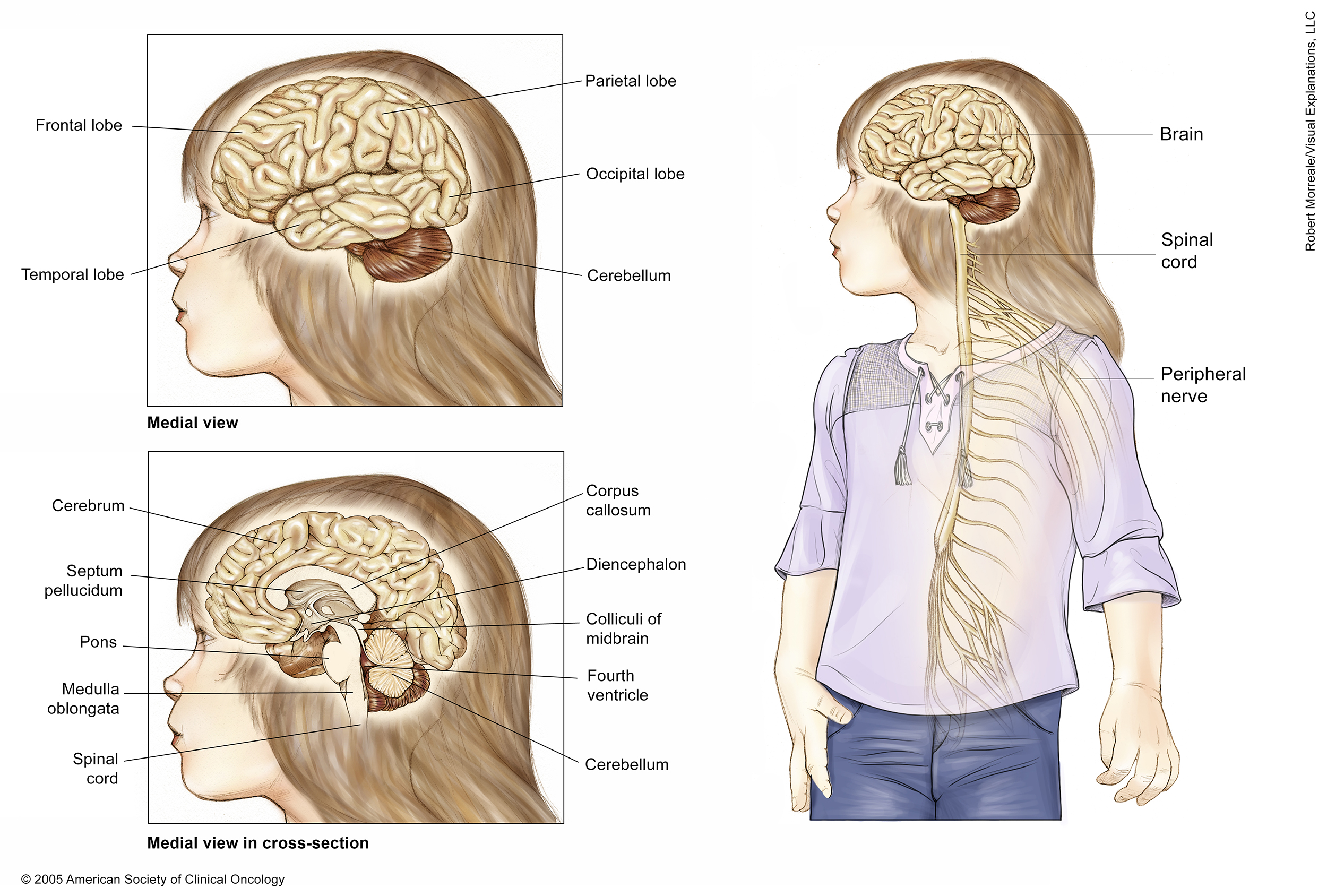

These illustrations show several views of a child’s brain and central nervous system. A medial (side) view of the brain shows the cerebrum and cerebellum. The cerebrum is the largest part of the brain and made up of 4 lobes: the frontal lobe at the front of the skull, the parietal lobe at the upper rear of the skull (above the occipital lobe), and the temporal lobe, which is located under the frontal and parietal lobes on both sides of the cerebrum. The cerebellum is located under the occipital and temporal lobes at the rear of the skull.
The cross section of the brain shows the long corpus callosum located under the cerebrum in the center of the brain, the septum pellucidum, which runs down from the corpus callosum, and the diencephalon, which connects the cerebrum and the brain stem. The brain stem is the lowest part of the brain. It is made up of 3 parts: the medulla oblongata, which connects to the spinal cord; the pons, which bulges out from the medulla oblongata; and the midbrain. The fourth ventricle is a fluid-filled space between the brain stem and the cerebellum, underneath the colliculi of the midbrain.
An overall view of the body shows that the spinal cord extends from the brain stem down the back. Peripheral nerves branch out from the spinal cord to the rest of the body.
Copyright 2004 American Society of Clinical Oncology. Robert Morreale/Visual Explanations, LLC.
The next section in this guide is Risk Factors . It describes the factors that may increase the chance of developing astrocytoma. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Risk Factors
ON THIS PAGE: You will find out more about the factors that increase the chance of developing astrocytoma. Use the menu to see other pages.
A risk factor is anything that increases a person’s chance of developing a tumor. Although risk factors often influence the development of a tumor, most do not directly cause a tumor. Some people with several risk factors never develop a tumor, while others with no known risk factors do.
Doctors and researchers do not know what causes most childhood tumors. There is some evidence that genetics may play a role in a small percentage of children with cerebral astrocytoma. The following factors may increase a child’s risk of developing astrocytoma:
-
Neurofibromatosis. Neurofibromatosis is an inherited disorder that causes a type of noncancerous tumor called a neurofibroma. Neurofibromatosis is also called Recklinghausen’s disease or von Recklinghausen’s disease. Learn more about neurofibromatosis type 1 and neurofibromatosis type 2 .
-
Other genetic conditions. Less commonly, the following genetic conditions are associated with a higher risk of developing a central nervous system (CNS) tumor:
-
Li-Fraumeni syndrome
-
Tuberous sclerosis complex
-
Nevoid basal cell carcinoma syndrome
-
Turcot syndrome
-
Constitutional mismatch repair deficiency syndrome (CMMRDS)
-
The next section in this guide is Symptoms and Signs . It explains what changes or medical problems astrocytoma can cause. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Symptoms and Signs
ON THIS PAGE : You will find out more about changes and other things that can signal a problem that may need medical care. Use the menu to see other pages.
Children with astrocytoma may experience the following symptoms or signs. Symptoms are changes that you can feel in your body. Signs are changes in something measured, like by taking your blood pressure or doing a lab test. Together, symptoms and signs can help describe a medical problem. Sometimes, children with astrocytoma do not have any of the symptoms and signs described below. Or, the cause of a symptom or sign may be a medical condition that is not a tumor.
-
Headaches
-
Feeling tired and listless
-
Seizures not related to a high fever
-
Eyesight problems, such as double vision
-
Changed growth or development
In a baby, the only symptom may be that their head is growing too fast. An infant’s skull can expand to make room for a growing tumor in the brain. So, a baby with astrocytoma may have a larger than expected head.
If you are concerned about any changes your child experiences, please talk with your child’s doctor. The doctor will ask how long and how often your child has been experiencing the symptom(s), in addition to other questions. This is to help figure out the cause of the problem, called a diagnosis .
If a tumor is diagnosed, relieving symptoms remains an important part of care and treatment. Managing symptoms may also be called "palliative care" or "supportive care." It is often started soon after diagnosis and continued throughout treatment. Be sure to talk with your child's health care team about the symptoms your child experiences, including any new symptoms or a change in symptoms.
The next section in this guide is Diagnosis . It explains what tests may be needed to learn more about the cause of the symptoms. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Diagnosis
ON THIS PAGE: You will find a list of common tests, procedures, and scans that doctors use to find the cause of a medical problem. Use the menu to see other pages.
Doctors use many tests to find, or diagnose, astrocytoma. They also do tests to learn if the tumor has spread to another part of the body from where it started. If the tumor has spread, it is called metastasis. Doctors may also do tests to learn which treatments could work best.
For most tumor types, a biopsy is the only sure way for the doctor to know if an area of the body has a tumor. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis.
How astrocytoma is diagnosed
There are many tests used for diagnosing astrocytoma. Not all tests described here will be used for every person. Your child’s doctor may consider these factors when choosing a diagnostic test:
-
The type of tumor suspected
-
Your child’s signs and symptoms
-
Your child’s age and general health
-
The results of earlier medical tests
In addition to a physical examination, the following tests may be used to diagnose astrocytoma:
-
Computed tomography (CT or CAT) scan. A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows any abnormalities or tumors. A CT scan can be used to measure the tumor’s size. Sometimes, a special dye called a contrast medium is given before the scan to provide better detail on the image. This dye can be injected into a patient’s vein or given as a pill to swallow.
-
Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. MRI can be used to measure the tumor’s size. A contrast medium is given before the scan to create a clearer picture. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow.
-
Biopsy. Other tests can suggest that a tumor is present, but only a biopsy can make a definite diagnosis. For astrocytoma, a biopsy is done to determine the type and grade of the tumor. It can also be used to identify certain molecular features that help the doctor plan treatment (see below). During a biopsy, a doctor called a neurosurgeon will remove a small piece of tissue from the tumor. A neurosurgeon specializes in treating a central nervous system (CNS) tumor using surgery. A pathologist then analyzes the sample. A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease.
-
Biomarker testing of the tumor. Your child's doctor may recommend running laboratory tests on a tumor sample to identify specific genes, proteins, and other factors unique to the tumor. This may also be called molecular testing of the tumor. Results of these tests can help determine your child’s treatment options (see Types of Treatment ).
After diagnostic tests are done, your child’s doctor will review the results with you. If the diagnosis is astrocytoma, these results also help the doctor describe the tumor. This is called staging and grading.
The next section in this guide is Stages and Grades . It explains the system doctors use to describe the extent of astrocytoma. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Stages and Grades
ON THIS PAGE: You will learn about how doctors describe astrocytoma’s growth or spread. This is called the stage or grade. Use the menu to see other pages.
What is staging?
Staging is a way of describing where a tumor is located, if or where it has spread, and whether it is affecting other parts of the body. Several types of childhood central nervous system (CNS) tumors can spread through the spinal fluid that surrounds the brain and the spine. This information helps the doctor recommend the best kind of treatment and helps predict the child's prognosis, which is the chance of recovery.
Grade
In addition to staging, doctors also describe astrocytoma by its grade. The grade describes how much tumor cells look like healthy cells when viewed under a microscope.
The doctor compares the tumor tissue with healthy tissue. Healthy tissue usually contains many different types of cells grouped together. If the tumor tissue looks similar to healthy tissue and has different cell groupings, it is called "differentiated" or a "low-grade tumor." If the tumor tissue looks very different from healthy tissue, it is called "poorly differentiated" or a "high-grade tumor." The tumor’s grade may help the doctor predict how quickly it will spread. In general, the lower the tumor’s grade, the better the prognosis.
The grades of astrocytoma are:
-
Low-grade tumor. A low-grade tumor has cells that look similar to healthy CNS cells under a microscope. The tumor usually does not grow quickly or spread to other parts of the CNS. However, the tumor can sometimes grow and spread quickly. Tumors may appear in multiple spots in the brain, especially when the disease is linked with neurofibromatosis (see Risk Factors ). Common low-grade tumors in children include juvenile pilocytic astrocytoma, or JPA, and diffuse astrocytoma.
-
High-grade tumor. A high-grade tumor has cells that do not look similar to healthy astrocytes. This type of tumor grows quickly and can spread throughout the CNS. Anaplastic astrocytoma is considered a high-grade tumor.
-
Recurrent astrocytoma. Recurrent astrocytoma is a tumor that has come back after treatment. If it returns, astrocytoma usually recurs near where it first started. If the tumor comes back, there will be another round of tests to learn about the extent of the recurrence. These tests and scans are often similar to those done at the time of the original diagnosis .
Information about the tumor’s grade and stage will help the doctor recommend a specific treatment plan. The next section in this guide is Types of Treatment . Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Types of Treatment
ON THIS PAGE: You will learn about the different types of treatments doctors use for children with astrocytoma. Use the menu to see other pages.
In general, tumors in children are uncommon. This means it can be hard for doctors to plan treatments unless they know what has been most effective in other children. That is why more than 60% of children are treated as part of a clinical trial. A clinical trial is a research study that tests a new approach to treatment. The “standard of care” is the best treatments known based on previous clinical trials. Clinical trials may test such approaches as a new drug, a new combination of existing treatments, or new doses of current therapies. The health and safety of all children participating in clinical trials are closely monitored.
To take advantage of these newer treatments, children with a central nervous system (CNS) tumor should be treated at a specialized cancer center. Doctors at these centers have extensive experience in treating children and have access to the latest research. A doctor who specializes in treating children with a tumor is called a pediatric oncologist. For astrocytoma, a neuro-oncologist may also be involved with treatment. This is a doctor who specializes in CNS tumors. If a pediatric cancer center is not nearby, general cancer centers sometimes have pediatric and neurology specialists who are able to be part of your child’s care.
How astrocytoma is treated
In many cases, a team of doctors works with a child and their family to provide care. This is called a multidisciplinary team . Pediatric cancer centers often have extra support services for children and their families, such as child life specialists, dietitians, physical and occupational therapists, social workers, and counselors. Special activities and programs to help your child and family cope may also be available.
Treatment options and recommendations depend on several factors, including the type and grade of the tumor, possible side effects, the family’s preferences, and the child’s overall health. Take time to learn about all of your child’s treatment options and be sure to ask questions about things that are unclear. Talk with your child’s doctor about the goals of each treatment and what you can expect during the treatment. These types of talks are called "shared decision-making." Shared decision-making is when you and your doctors work together to choose treatments that fit the goals of your child's care. Shared decision-making is particularly important for astrocytoma because there are different treatment options. Learn more about making treatment decisions .
The common types of treatments used for astrocytoma are described below, including treatments called targeted therapy and immunotherapy that may be available through clinical trials. Your child’s care plan also includes treatment for symptoms and side effects, an important part of your child's medical care.
-
Surgery
-
Radiation therapy
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
-
Physical, emotional, and social effects of a CNS tumor
-
Remission and the chance of recurrence
-
If treatment does not work
Surgery
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. It is the most common treatment for astrocytoma. During surgery, a neurosurgeon removes as much of the tumor as possible.
Sometimes, a tumor is inoperable, meaning it cannot be reached by surgery because of its location. However, even for inoperable tumors, a surgical biopsy can usually still be done to find out the type and grade of the tumor (see
Diagnosis
).
If a low-grade tumor cannot be completely removed, the doctor usually watches for signs of tumor growth before recommending other types of treatment. If a tumor causes symptoms and cannot be completely removed with surgery, radiation therapy or chemotherapy is often used (see "Radiation therapy" and "Chemotherapy," below).
A child with a high-grade tumor often needs additional treatment regardless of whether the entire tumor was removed during surgery.
Before surgery, talk with your child’s health care team about the possible side effects from the recommended surgery and how side effects can be managed. Learn more about the basics of surgery .
Return to top
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy tumor cells. A doctor who specializes in giving radiation therapy to treat a tumor is called a radiation oncologist.
The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. When radiation treatment is given using implants, it is called internal radiation therapy or brachytherapy. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
Side effects from radiation therapy may include fatigue, mild skin reactions, upset stomach, and loose bowel movements. Most short-term side effects go away soon after treatment is finished.
Radiation therapy can sometimes cause problems with the long-term growth and development of a child’s brain. This means that the doctor may choose to treat the tumor in another way. To avoid or reduce the need for radiation therapy in young children, the doctor may first use chemotherapy (see below) to shrink the tumor.
Learn more about the basics of radiation therapy .
Return to top
Therapies using medication
The treatment plan may include medications to destroy tumor cells. Medication may be given through the bloodstream to reach tumor cells throughout the body. When a drug is given this way, it is called systemic therapy. Medication may also be given locally, which is when the medication is applied directly to the tumor or kept in a single part of the body.
This treatment is generally prescribed by a medical oncologist, a doctor who specializes in treating a tumor with medication.
Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications, be sure to ask your health care team about how to safely store and handle them.
The types of medications used for astrocytoma include:
-
Chemotherapy
-
Targeted therapy
-
Immunotherapy
Each of these types of therapies is discussed below in more detail. A person may receive 1 type of medication at a time or a combination of medications given at the same time. They can also be given as part of a treatment plan that includes surgery and/or radiation therapy.
The medications used to treat astrocytoma are continually being evaluated. Talking with your child’s doctor is often the best way to learn about the medications prescribed for your child, their purpose, and their potential side effects or interactions with other medications.
It is also important to let your doctor know if your child is taking any other prescription or over-the-counter medications or supplements. Herbs, supplements, and other drugs can interact with anti-tumor medications, causing unwanted side effects or reduced effectiveness. Learn more about your child’s prescriptions by using searchable drug databases .
Chemotherapy
Chemotherapy is the use of drugs to destroy tumor cells, usually by keeping the tumor cells from growing, dividing, and making more cells.
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. A patient may receive a single drug at a time or combinations of different drugs given at the same time. Chemotherapy for astrocytoma often involves a combination of 2 or 3 drugs.
Chemotherapy may be used to delay or avoid using radiation therapy in young children with low-grade tumors, such as juvenile pilocytic astrocytoma (JPA), due to possible side effects. For a high-grade tumor, chemotherapy may work better when combined with surgery and radiation therapy.
The side effects of chemotherapy depend on the individual and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away after treatment is finished. Talk with your child's doctor about what to expect based on the specific medications prescribed.
Learn more about the basics of chemotherapy .
Return to top
Targeted therapy
Targeted therapy is a treatment that targets the tumor’s specific genes, proteins, or the tissue environment that contributes to the tumor’s growth and survival. This type of treatment blocks the growth and spread of tumor cells and limits damage to healthy cells.
Not all tumors have the same targets. To find the most effective treatment, your child’s doctor may run tests to identify the genes, proteins, and other factors in the tumor. This helps doctors better match each child with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments .
Larotrectinib (Vitrakvi) is a type of targeted therapy that is not specific to a certain type of tumor but focuses on a specific genetic change called an NTRK fusion. This is also called a tumor-agnostic treatment . NTRK fusions are found in a range of tumors, including astrocytoma. Larotrectinib is approved as a treatment for astrocytoma that is metastatic or cannot be removed with surgery and has worsened despite other treatments.
Talk with your child’s doctor to learn more about targeted treatment options within a clinical trial . In addition, ask about possible side effects for a specific medication and how they can be managed.
Return to top
Immunotherapy
Immunotherapy uses the body's natural defenses to fight a tumor by improving your immune system’s ability to attack tumor cells.
Immunotherapy for astrocytoma is currently being researched in clinical trials . Talk with your child’s doctor to learn more about treatment options within a clinical trial.
Different types of immunotherapy can cause different side effects. Common side effects include skin reactions, flu-like symptoms, diarrhea, and weight changes. Talk with your child’s doctor about possible side effects for the immunotherapy recommended for your child. Learn more about the basics of immunotherapy .
Return to top
Physical, emotional, and social effects of a CNS tumor
A CNS tumor and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your child’s care that is included along with treatments intended to slow, stop, or eliminate the tumor.
Supportive care focuses on improving how your child feels during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of the tumor, may receive this type of care. And it often works best when it is started right after a CNS tumor diagnosis. People who receive palliative care along with treatment for the tumor often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Supportive care can vary widely and often includes medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. Your child may also receive palliative treatments similar to those meant to get rid of the tumor, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your child’s doctor about the goals of each treatment in the recommended treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options. Many patients also benefit from talking with a social worker and participating in support groups. Ask your doctor about these resources, too.
During treatment, your child’s health care team may ask you to answer questions about your child’s symptoms and side effects and to describe each problem. Be sure to tell the health care team if your child is experiencing a problem. This helps the health care team treat any symptoms and side effects as quickly as possible. It can also help prevent more serious problems in the future.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Return to top
Remission and the chance of recurrence
A remission is when tumor cells cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
A remission may be temporary or permanent. This uncertainty causes many people to worry that the tumor will come back. While many remissions are permanent, it is important to talk with your child's doctor about the possibility of the disease returning. Understanding your child’s risk of recurrence and the treatment options may help you feel more prepared if the tumor does return. Learn more about coping with the fear of recurrence .
If the tumor returns after the original treatment, it is called a recurrent tumor. It may come back in the same place (called a local recurrence), nearby (regional recurrence), or in another place (distant recurrence). When astrocytoma recurs, it usually recurs near where the tumor originally started.
If a recurrence happens, a new cycle of testing will begin again to learn as much as possible about it. After this testing is done, you and your child’s doctor will talk about the treatment options. Often the treatment plan will include the treatments described above, such as surgery, radiation therapy, and therapies using medication, but they may be used in a different combination or given at a different pace. Your child’s doctor may suggest clinical trials that are studying new ways to treat recurrent astrocytoma. Whichever treatment plan you choose, palliative care will be important for relieving symptoms and side effects.
Treatment for recurrent astrocytoma depends on 3 factors:
-
Grade of the tumor
-
Where the tumor recurred
-
The type of treatment your child received for the original tumor
If the tumor is a low-grade recurrent astrocytoma, the doctor may perform surgery to remove as much of the tumor as possible. Children who have not previously had radiation therapy or chemotherapy may receive either or both of these treatments for the recurrent tumor.
If the tumor is a high-grade recurrent astrocytoma, the doctor may suggest other types of chemotherapy or radiation therapy. Rarely, chemotherapy along with stem cell/bone marrow transplantation may be recommended.
A recurrent tumor may bring up emotions such as disbelief or fear. You and your family are encouraged to talk with your child's health care team about these feelings and ask about support services to help you cope. Learn more about dealing with a recurrence .
Return to top
If treatment does not work
Although treatment is successful for many children with a CNS tumor, sometimes it is not. If a child’s tumor cannot be cured or controlled, this is called an advanced or terminal tumor. This diagnosis is stressful, and an advanced tumor may be difficult to discuss. However, it is important to have open and honest conversations with your child’s health care team to express your family’s feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help.
Hospice care is designed to provide the best possible quality of life for people who are expected to live less than 6 months. Parents and guardians are encouraged to talk with the health care team about hospice options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment can make staying at home a workable option for many families. Some children may be happier and more comfortable if they can attend school part-time or keep up other activities and social connections. The child’s health care team can help parents or guardians decide on an appropriate level of activity. Making sure a child is physically comfortable and free from pain is extremely important as part of end-of-life care. Learn more about caring for a terminally ill child and advanced care planning .
The death of a child is an enormous tragedy, and families may need support to help them cope with the loss. Pediatric cancer centers often have professional staff and support groups to help with the process of grieving. Learn more on grieving the loss of a child .
Return to top
The next section in this guide is About Clinical Trials . It offers more information about research studies that are focused on finding better ways to care for children with astrocytoma. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - About Clinical Trials
ON THIS PAGE: You will learn more about clinical trials, which are the main way that new medical approaches are studied to see how well they work. Use the menu to see other pages.
What are clinical trials?
Doctors and scientists are always looking for better ways to care for children with astrocytoma. To make scientific advances, doctors create research studies involving volunteers, called clinical trials. Every drug that is now approved by the U.S. Food and Drug Administration (FDA) was tested in clinical trials.
Clinical trials are used for all types and stages of astrocytoma. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of existing treatments, new approaches to radiation therapy or surgery, and new methods of treatment.
Children who participate in clinical trials can be some of the first to get a treatment before it is available to the public. However, there are some risks with a clinical trial, including possible side effects and the chance that the new treatment may not work. People are encouraged to talk with their child’s health care team about the pros and cons of joining a specific study.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment. Talk with your child’s doctor about clinical trials for symptoms and side effects.
Deciding to join a clinical trial
People decide to participate in clinical trials for many reasons. For some, a clinical trial is the best treatment option available. Because standard treatments are not perfect, patients are often willing to face the added uncertainty of a clinical trial in the hope of a better result. Others volunteer for clinical trials because they know that these studies are a way to contribute to the progress in treating astrocytoma. Even if they do not benefit directly from the clinical trial, their participation may benefit future children with astrocytoma.
Insurance coverage and the costs of clinical trials differ by location and by study. In some programs, some of the expenses from participating in the clinical trial are reimbursed. In others, they are not. It is important to talk with the research team and your insurance company first to learn if and how treatment in a clinical trial will be covered. Learn more about health insurance coverage of clinical trials .
Sometimes people have concerns that, in a clinical trial, their child may receive no treatment by being given a placebo or a “sugar pill.” You and your child will always be told when a placebo is used in a study. Find out more about placebos in cancer clinical trials .
Patient safety and informed consent
To join a clinical trial, parents and children must participate in a process known as informed consent. Informed consent means that parents give permission for their child to participate in a clinical trial and that teenagers give their consent to participate. During informed consent, the doctor should:
-
Describe all of the treatment options, so that the person understands how the new treatment differs from the standard treatment.
-
List all of the risks of the new treatment, which may or may not be different from the risks of standard treatment.
-
Explain what will be required of each person in order to participate in the clinical trial, including the number of doctor visits, tests, and the schedule of treatment.
-
Describe the purposes of the clinical trial and what researchers are trying to learn.
Clinical trials also have certain rules called “eligibility criteria” that help structure the research and keep patients safe. You and the research team will carefully review these criteria together. Your child will need to meet all of the eligibility criteria in order to participate in a clinical trial. Learn more about eligibility criteria in clinical trials.
People who participate in a clinical trial may stop participating at any time for personal or medical reasons. This may include that the new treatment is not working or there are serious side effects. Clinical trials are also closely monitored by experts who watch for any problems with each study. It is important that parents talk with the doctor and researchers about who will be providing their child’s treatment and care during the clinical trial, after the clinical trial ends, and/or if they choose to leave the clinical trial before it ends.
Finding a clinical trial
Research through clinical trials is ongoing for all types of tumors. For specific topics being studied for astrocytoma, learn more in the Latest Research section.
Cancer.Net offers more information about clinical trials in other areas of the website, including a complete section on clinical trials and places to search for clinical trials for a specific type of tumor .
In addition, you can find a free video-based educational program about cancer clinical trials located in another section of this website.
The next section in this guide is Latest Research . It explains areas of scientific research for astrocytoma. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Latest Research
ON THIS PAGE: You will read about the scientific research being done to learn more about astrocytoma and how to treat it. Use the menu to see other pages.
Doctors are working to learn more about astrocytoma. This includes ways to prevent it and how to provide the best care to children diagnosed with astrocytoma. The following areas of research may include new options for patients through clinical trials. Always talk with your child’s doctor about the best diagnostic and treatment options for your child.
-
Improved methods of imaging and surgery. Imaging techniques are being developed and improved that help surgeons better pinpoint the tumor’s location. These techniques can help reduce or prevent damage to the healthy parts of the central nervous system (CNS) during treatment.
-
Functional magnetic resonance imaging (fMRI) identifies the parts of the brain that control speech, hearing, vision, touch, and movement. The specific locations of these functions are slightly different in each person. Functional MRI allows surgeons to plan surgery around these areas.
-
Image-guided stereotaxis allows surgeons to visualize and operate on the brain using 3-dimensional outlines of the brain and the tumor. Along with specialized software, these images help guide the surgeon to the tumor. Tumors that were once considered inoperable can often be removed with this technique.
-
-
Improved ways to give radiation therapy. Conformal radiation therapy is a way to deliver high doses of radiation directly to a tumor and not healthy tissue. This technique produces detailed 3-dimensional maps of the brain and tumor. These maps help doctors know exactly where to direct the radiation therapy.
-
Targeted treatments based on the tumor's molecular features. As discussed in Types of Treatment , researchers are studying the use of targeted therapy to treat astrocytoma with certain genetic changes. Specifically, researchers are studying new drugs that target changes, called mutations or alterations, on the BRAF gene.
-
Immunotherapy. As outlined in Types of Treatment , immunotherapy is an active area of research for astrocytoma. Researchers are studying how well these types of drugs work and how safe they are for children with both high-grade and low-grade astrocytoma.
-
Palliative care/supportive care. Clinical trials are underway to find better ways of reducing symptoms and side effects of current astrocytoma treatments to improve comfort and quality of life for patients.
Looking for More About the Latest Research?
If you would like more information about the latest areas of research in childhood CNS tumors, explore these related items that take you outside of this guide:
-
To find clinical trials specific to the diagnosis, talk with your child’s doctor or search online clinical trial databases .
-
Visit the website of Conquer Cancer, the ASCO Foundation , to find out how to help support cancer research. Please note that this link takes you to a different ASCO website.
The next section in this guide is Coping with Treatment . It offers some guidance on how to cope with the physical, emotional, social, and financial changes that astrocytoma and its treatment can bring. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Coping with Treatment
ON THIS PAGE: You will learn more about coping with the physical, emotional, social, and financial effects of astrocytoma and its treatment. Use the menu to see other pages.
Every treatment for astrocytoma can cause side effects or changes to your child’s body and how they feel. For many reasons, children do not experience the same side effects even when given the same treatment. This can make it hard to predict how your child will feel during treatment.
As your child prepares to start treatment, it is normal to fear treatment-related side effects . It may help to know that your child’s health care team will work to prevent and relieve side effects. This part of treatment is called palliative care or supportive care. It is an important part of your child’s treatment plan, regardless of their age or the stage of disease.
Coping with physical side effects
Common physical side effects from each treatment option for astrocytoma are described in the Types of Treatment section. Learn more about side effects of tumors and their treatment, along with ways to prevent or control them . Changes to your child’s physical health depend on several factors, including the tumor’s stage and grade, the length and dose of treatment, and your child’s general health.
It is important to discuss any new side effects or changes in existing side effects with your child’s health care team. Providing this information helps them find ways to treat or manage the side effects so your child feels more comfortable and can potentially keep any side effects from worsening.
You may find it helpful to keep track of your child’s side effects so you are prepared to discuss any changes with the health care team. Learn more about why tracking side effects is helpful .
Sometimes, side effects can last after treatment ends. Doctors call these long-term side effects. Side effects that occur months or years after treatment are called late effects . Treating long-term side effects and late effects is an important part of survivorship care. Learn more by reading the Follow-Up Care section of this guide or talking with your child’s doctor.
Coping with emotional and social effects
Your family can have emotional and social effects after a diagnosis of astrocytoma. This may include dealing with a variety of emotions, such as anxiety, sadness, or anger, or managing stress. Sometimes, people find it difficult to express how they feel to their loved ones. Some have found that talking to an oncology social worker, counselor, or member of the clergy can help them develop more effective ways of coping and talking about the diagnosis.
You can also find coping strategies for emotional and social effects in a separate section of this website. This section includes many resources for finding support and information to meet your family's needs.
Coping with the costs of medical care
Treatment for astrocytoma can be expensive. It can be a source of stress and anxiety for families. In addition to treatment costs, many people find they have extra, unplanned expenses related to their child’s care. Families are encouraged to talk about financial concerns with a member of their health care team. Learn more about managing financial considerations in a separate part of this website.
Coping with barriers to care
Some groups of people experience different rates of new tumor cases and experience different outcomes from their diagnosis. These differences are called “cancer disparities.” Disparities are caused in part by real-world barriers to quality medical care and social determinants of health , such as where a person lives and whether they have access to food and health care. Cancer disparities more often negatively affect racial and ethnic minorities , poor people , sexual and gender minorities (LGBTQ+) , adolescent and young adult populations , older adults , and people who live in rural areas or other underserved communities .
If your child is having difficulty getting the care they need, talk with a member of the health care team or explore other resources that help support medically underserved people .
Talking with your child's health care team about side effects
Before starting treatment, talk with your child’s doctor about possible side effects. Ask:
-
Which side effects are most likely?
-
When are they likely to happen?
-
What can we do to prevent or relieve them?
-
When and who should we call about side effects?
Be sure to tell your child’s health care team about any side effects that happen during treatment and afterward, too. Tell them even if you do not think the side effects are serious. This discussion should include physical, emotional, social, and financial effects.
Caring for a child with astrocytoma
Family members and friends often play an important role in taking care of a child with astrocytoma. This is called being a caregiver. As a parent or guardian, you are the primary caregiver for your child. However, friends and family can give you valuable support, even if they live far away.
When your child has astrocytoma, you may have an additional range of responsibilities. These may include giving medications or managing symptoms and side effects. However, it is important to seek help from others. Below are some of the responsibilities your family or friends could help with:
-
Providing short-term care for your child
-
Giving support and encouragement
-
Assisting with meals or household chores
-
Helping with insurance and billing issues
A caregiving plan can help caregivers stay organized and help identify opportunities to delegate tasks to others. Ask how much care your child may need at home and with daily tasks during and after treatment. Use this 1-page fact sheet that includes an action plan to help make caregiving a team effort. This free fact sheet is available as a PDF, so it is easy to print.
Learn more about caregiving or read the ASCO Answers Guide to Caring for a Loved One With Cancer in English or Spanish .
Looking for More on How to Track Side Effects?
Cancer.Net offers several resources to help you keep track of symptoms and side effects. Please note that these links will take you to other sections of Cancer.Net:
-
Cancer.Net Mobile: The free Cancer.Net mobile app allows you to securely record the time and severity of your child's symptoms and side effects.
-
ASCO Answers Managing Pain: Get this 32-page booklet about the importance of pain relief that includes a pain tracking sheet to record how pain affects your child. The free booklet is available as a PDF, so it is easy to print.
-
ASCO Answers Fact Sheets: Read 1-page fact sheets on anxiety and depression , constipation , diarrhea , rash , and immunotherapy side effects that provide a tracking sheet to record details about the side effect. These free fact sheets are available as a PDF, so they are easy to print, fill out, and give to your child's health care team.
The next section in this guide is Follow-Up Care . It explains the importance of checkups after treatment for astrocytoma is finished. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Follow-Up Care
ON THIS PAGE:
You will read about your child’s medical care after treatment for astrocytoma is completed and why this follow-up care is important. Use the menu to see other pages.
Care for children diagnosed with astrocytoma does not end when active treatment has finished. Your child’s health care team will continue to check that the tumor has not come back, manage any side effects, and monitor your child’s overall health. This is called follow-up care. All children treated for a tumor, including astrocytoma, should have life-long, follow-up care.
Your child’s follow-up care may include regular physical examinations, medical tests, or both. Doctors want to keep track of your child’s recovery in the months and years ahead. A child’s specific follow-up care plan depends on many factors, including the grade of tumor and its location, the child’s age, and the type of treatment given.
Rehabilitation may be recommended, and this could mean any of a wide range of services such as physical therapy, family or individual counseling, nutritional planning, and/or educational assistance. The goal of rehabilitation is to help survivors and their families regain control over many aspects of their lives and remain as independent as possible. Learn more about this type of rehabilitation.
Learn more about the importance of follow-up care .
Watching for recurrence
One goal of follow-up care is to check for a recurrence, which means that the tumor has come back. A tumor recurs because small areas of tumor cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms.
During follow-up care, a doctor familiar with your child’s medical history can give you personalized information about the risk of recurrence. The doctor will ask specific questions about your child’s health. Some children may have blood tests or imaging tests as part of regular follow-up care, but testing recommendations depend on several factors, including the type, stage, and grade of the tumor first diagnosed and the types of treatment given.
The anticipation before having a follow-up test or waiting for test results may add stress to you or a family member. This is sometimes called “scanxiety.” Learn more about how to cope with this type of stress .
Managing long-term and late side effects of astrocytoma
Sometimes, side effects may linger beyond the active treatment period. These are called long-term side effects. In addition, other side effects called late effects may develop months or even years after treatment has ended. Late effects can occur almost anywhere in the body. They include physical problems, such as heart and lung problems, and second cancers, which is a new type of tumor that happens in someone who has had a tumor before. They also include emotional problems, such as anxiety and depression, and problems with memory, thinking, attention, and learning.
Based on the type of treatment your child received, the doctor will recommend examinations and tests to check for late effects.
-
Surgery. The risks and possible side effects vary widely, depending on the location and features of the tumor.
-
Chemotherapy. The risks and chance of secondary cancers are based on the specific drugs and doses.
-
Radiation therapy. Radiation therapy to the head and spine may cause cognitive and endocrine (hormonal) symptoms over time. The seriousness of these side effects depends on the dose and your child’s age.
Follow-up care should address your child’s quality of life, including any developmental or emotional concerns.
The Children's Oncology Group (COG) has studied the physical and psychological effects that childhood cancer survivors face. Based on these studies, COG has created long-term follow-up care recommendations for childhood, adolescent, and young adult survivors that can be found on a separate website:
www.survivorshipguidelines.org
.
Keeping a child’s personal health record
You are encouraged to organize and keep a personal record of your child’s medical information. The doctor will help you create this. That way, as your child enters adulthood, they have a clear, written history of the diagnosis, the treatments, and the doctor’s recommendations about the schedule for follow-up care. The American Society of Clinical Oncology (ASCO) offers forms to keep track of the treatment your child received and develop a survivorship care plan when treatment is completed.
Some children continue to see their oncologist, while others transition back to the care of their pediatrician, primary care doctor, or another health care professional. This decision depends on several factors, including the type, stage, and grade of the tumor, side effects, health insurance rules, and your family’s personal preferences. Talk with the health care team about your child’s ongoing medical care and any concerns you have about their future health.
If a doctor who was not directly involved in your child’s care for astrocytoma will lead the follow-up care, be sure to share the treatment summary and survivorship care plan forms with them and with all future health care providers. Details about the specific treatment given are very valuable to the health care professionals who will care for your child throughout their lifetime.
The
next section in this guide is Survivorship
. It describes how to cope with challenges in everyday life after a diagnosis of astrocytoma. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Survivorship
ON THIS PAGE: You will read about how to cope with challenges in everyday life after your child’s diagnosis. Use the menu to see other pages.
What is survivorship?
The word “survivorship” means different things to different people, but it often describes living with, through, and beyond the diagnosis of a central nervous system (CNS) tumor. In some ways, survivorship is one of the most complicated parts of the experience because it is different for every child and their family.
After active treatment for astrocytoma ends, children and their families may experience a mixture of strong feelings, including joy, concern, relief, guilt, and fear. Some people say they appreciate life more after the diagnosis. Other families stay very anxious about their child’s health and become uncertain about coping with everyday life.
One source of stress may occur when frequent visits to the health care team end after completing treatment. Often, relationships built with the health care team provide a sense of security during treatment, and children and their families miss this source of support. This may be especially true when new worries and challenges surface over time, such as any late effects of treatment, learning or school problems, emotional challenges, sexual development and fertility concerns, and/or financial issues.
Every family faces different concerns and challenges. With any challenge, a good first step is being able to recognize each fear and talk about it. Effective coping requires:
-
Understanding the challenge your family is facing
-
Thinking through solutions
-
Asking for and allowing the support of others
-
Feeling comfortable with the course of action your family chooses
It may be helpful to join an in-person support group or online community of childhood CNS tumor survivors. Support groups also exist for parents of children diagnosed with a CNS tumor. This allows you to talk with people who have had similar first-hand experiences. Other options for finding support include talking with a friend or member of the health care team, individual counseling, or asking for assistance at the learning resource center of the place where your child received treatment.
Healthy living after astrocytoma
Survivorship often serves as a strong motivator to make lifestyle changes, often for the whole family.
Children who have had astrocytoma can enhance the quality of their future by following established guidelines for good health into and through adulthood, including not smoking, limiting alcohol, maintaining a healthy weight, eating well, managing stress, and participating in regular physical activity. Talk with the doctor about developing a plan that is best for your child’s needs. Learn more about making healthy lifestyle choices .
It is important that your child has recommended medical checkups and tests (see Follow-Up Care ) to take care of their health.
Talk with the doctor to develop a survivorship care plan that is best for your child’s needs.
Changing role of caregivers
Parents, other family members, and friends may also go through periods of transition. A caregiver plays a very important role in supporting a child diagnosed with astrocytoma, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver's role often changes. Eventually, the need for caregiving related to a child’s diagnosis will become much less or come to an end as your child gets older. Family counselors at pediatric cancer centers can help with this transition. You can also learn more about adjusting to life after caregiving .
Looking for More Survivorship Resources?
For more information about survivorship, explore these related items. Please note these links will take you to other sections of Cancer.Net:
-
Survivorship Resources : Cancer.Net offers information and resources to help survivors cope, including specific sections for children and teens and young adults . There is also a main section on survivorship for people of all ages.
-
ASCO Answers Guide to Cancer Survivorship: Get this 48-page booklet that helps people transition into life after treatment. It includes a blank treatment summary and survivorship care plan forms. The free booklet is available as a PDF, so it is easy to print.
The next section offers Questions to Ask the Health Care Team to help start conversations with your child’s medical care team. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Questions to Ask the Health Care Team
ON THIS PAGE: You will find some questions to ask your child’s medical care team, to help you better understand your child’s diagnosis, treatment plan, and overall care. Use the menu to see other pages.
Talking often with your child's health care team is important to make informed decisions about your child’s health care. These suggested questions are a starting point to help you learn more about your child’s care and treatment. You are also encouraged to ask additional questions that are important to you. You may want to print this list and bring it to your child’s next appointment, or download Cancer.Net’s free mobile app for a digital list and other interactive tools to manage your child’s care. It may also be helpful to ask a family member or friend to come with you to appointments to help take notes.
Questions to ask after getting a diagnosis
-
Where exactly is the astrocytoma located?
-
What is the grade of the tumor? What does this mean?
-
What is your familiarity with my child’s tumor type and its treatment?
-
Can you explain my child’s pathology report (laboratory test results) to me?
Questions to ask about choosing a treatment and managing side effects
-
What treatment options are available?
-
Are there other treatment options available at other cancer centers?
-
What clinical trials are available for my child? Where are they located, and how do I find out more about them?
-
What treatment plan do you recommend? Why?
-
What is the goal of each treatment? Is it to eliminate the tumor, help my child feel better, or both?
-
Who will be part of my child’s health care team, and what does each member do?
-
Who will be leading my child’s overall treatment?
-
What are the possible side effects of this treatment?
-
How will this treatment affect my child’s daily life? Will they be able to go to school and perform their usual activities?
-
Could this treatment affect my child’s ability to become pregnant or have children in the future? If so, should I talk with a fertility specialist before treatment begins?
-
If I’m worried about managing the costs of medical care, who can help me?
-
What support services are available to my child? To my family?
-
If I have questions or problems, who should I call?
Questions to ask about surgery
-
What type of surgery will my child have?
-
How long will the operation take?
-
How long will my child be in the hospital?
-
Can you describe what recovery from surgery will be like?
-
Who should I contact about any side effects my child experiences? And how soon?
-
What are the possible long-term effects of surgery?
Questions to ask about radiation therapy
-
What type of treatment is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
Will my child receive this treatment at a hospital or clinic?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects my child experiences? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about chemotherapy, targeted therapy, and immunotherapy
-
What type of treatment is recommended?
-
What is the goal of this treatment?
-
How long will it take to give this treatment?
-
Will my child receive this treatment at a hospital or clinic? Or will they take it at home?
-
What side effects can I expect during treatment?
-
Who should I contact about any side effects my child experiences? And how soon?
-
What are the possible long-term or late effects of having this treatment?
-
What can be done to prevent or relieve the side effects?
Questions to ask about planning follow-up care
-
What is the chance that the tumor will come back? Should I watch for specific signs or symptoms?
-
What long-term side effects or late effects are possible based on the treatment my child received?
-
What follow-up tests will my child need, and how often will those tests be needed?
-
How do I get a treatment summary and survivorship care plan to keep in my personal records?
-
Who will be leading my child’s follow-up care?
-
What survivorship support services are available to my child? To my family?
The next section in this guide is Additional Resources . It offers more resources on this website that may be helpful to you. Use the menu to choose a different section to read in this guide.
Astrocytoma - Childhood - Additional Resources
ON THIS PAGE: You will find some helpful links to other areas of Cancer.Net that provide information about medical care and treatment. This is the final page of Cancer.Net’s Guide to Childhood Astrocytoma. Use the menu to go back and see other pages.
Cancer.Net includes many other sections about the medical and emotional aspects of being diagnosed with a tumor for the patient and their family members and friends. This website is meant to be a resource for you and your loved ones from the time of diagnosis, through treatment, and beyond.
Here are a few links to help you explore other parts of Cancer.Net:
-
Search for a specialist in your local area using this free database of doctors from the American Society of Clinical Oncology (ASCO).
-
Learn what phrases and terms used in medical care and treatment mean.
-
Read more about the first steps to take when your child is diagnosed with a tumor .
-
Find out more about clinical trials as a treatment option.
-
Get information about managing the financial costs of medical care.
-
Learn more about coping with the emotions that a tumor can bring, including those within a family or a relationship.
-
Find a national, not-for-profit advocacy organization that may offer additional information, services, and support for children with astrocytoma.
-
Explore what to do when your child finishes active treatment .
-
Download Cancer.Net Mobile , a free app that includes a symptom and side effect tracker, medication reminders, and other interactive resources.
-
To find a range of information and insights from different voices on timely topics, visit the Cancer.Net Blog .
-
Watch Cancer.Net videos with ASCO experts explaining the basics of treatment, side effects, survivorship, clinical trials, caregiving, and more.
This is the end of the Cancer.Net’s Guide to Childhood Astrocytoma. Use the menu to choose a different section to read in this guide.













